Get the free healthspring appeal form
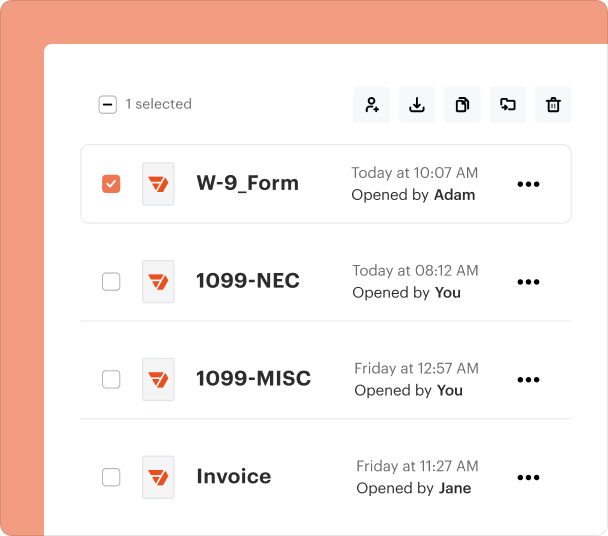
Fill out, sign, and share forms from a single PDF platform
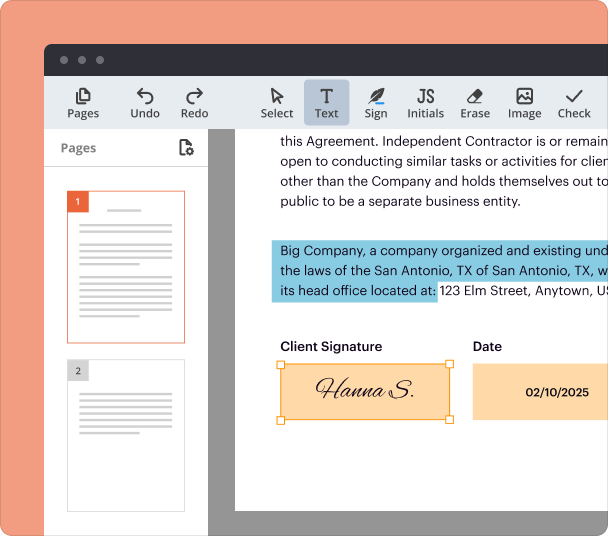
Edit and sign in one place
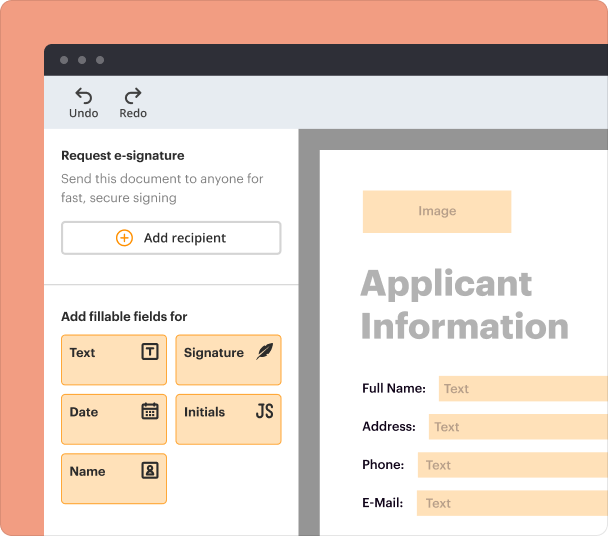
Create professional forms
Simplify data collection
Manage forms centrally
Why pdfFiller is the best tool for your documents and forms
End-to-end document management
Accessible from anywhere
Secure and compliant
Navigating the HealthSpring appeal process
How does the appeal process work for HealthSpring?
The HealthSpring appeal process enables individuals and their representatives to challenge adverse decisions made regarding healthcare coverage. In essence, an appeal is a formal request that disputes a decision affecting a member’s eligibility, benefits, or coverage. Understanding this process and utilizing the correct appeal form is critical to ensuring that healthcare needs are met effectively.
What is the appeal request?
An appeal in the context of HealthSpring is a formal way to contest decisions made about your care or coverage.
-
An appeal is a formal request to reconsider a decision made by HealthSpring regarding your health coverage.
-
Any HealthSpring member or their appointed representative can file an appeal.
-
The appeal process is vital for addressing adverse decisions, ensuring access to necessary healthcare services.
How should prepare to submit my appeal?
Preparation is crucial in the appeals process. Gathering necessary documentation and details before submission can enhance the likelihood of a favorable outcome.
-
Collect any relevant evidence to support your case, including medical records or payment histories.
-
Be clear about what decision you are appealing to tailor your appeal effectively.
-
If you choose to have representation, ensure they are well-informed about your case and healthcare needs.
How do complete the HealthSpring appeal form?
Filling out the HealthSpring appeal form correctly is vital for your appeal's success. The process can be simplified using tools like pdfFiller.
-
Follow each step on the pdfFiller platform to accurately complete your appeal form.
-
Ensure personal information and details about the adverse decision are correctly filled out to avoid delays.
-
Utilize features that allow easy edits, making the completion of your form more efficient.
What are the steps to submit my appeal?
After completing your appeal form, you'll need to submit it through the appropriate channels. This can also be easily done through pdfFiller.
-
Use pdfFiller to electronically sign your completed appeal form for a more efficient submission.
-
Choose between electronic submission via pdfFiller or mailing the form to the relevant HealthSpring address.
-
Monitor the progress of your appeal directly through pdfFiller, staying informed every step of the way.
What happens after submission?
Once your appeal is submitted, it enters a review process. Understanding what to expect can help you prepare for the next steps.
-
HealthSpring has a formalized process for reviewing appeals, which involves assessing submitted information.
-
Typically, you can expect to hear back within a specified period, but this can vary by case.
-
Appeals may be approved, denied, or require further information; understanding these outcomes can shape your next actions.
What are best practices for managing appeals?
Effective management of your appeal improves your chances of success. Using collaborative tools can streamline the process.
-
Engage with others involved in the appeal through pdfFiller’s collaboration features.
-
Keep all related documents and communications in a designated location for easy access.
-
Regularly follow up on your appeal to ensure it is receiving the necessary attention.
Frequently Asked Questions about cigna healthspring reconsideration form
What is an appeal in HealthSpring?
An appeal is a formal request to challenge a decision made regarding your healthcare coverage. It allows members to seek reconsideration based on specific criteria.
What documents do I need to submit an appeal?
You need to gather relevant medical records, payment histories, and any correspondence regarding the adverse decision to support your appeal.
Can a representative file an appeal on my behalf?
Yes, you can authorize a representative to submit an appeal for you. Make sure they are well-versed in your situation and healthcare needs.
How long will it take to get a response to my appeal?
Response times can vary, but many appeals are reviewed within 30 days. It is important to stay in touch with HealthSpring for updates.
What if my appeal is denied?
If your appeal is denied, you will receive a formal notification. At that point, you may consider options for further recourse or additional appeals.
pdfFiller scores top ratings on review platforms