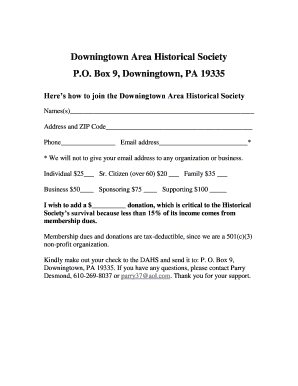
Get the free history and physical template form
Get, Create, Make and Sign
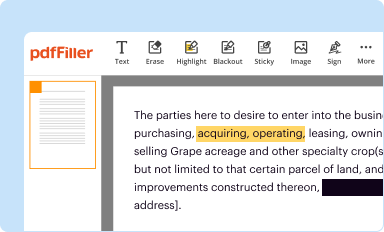
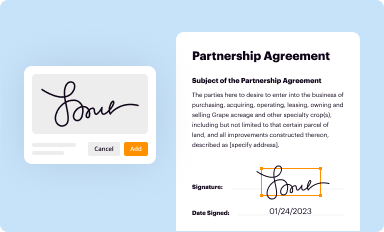
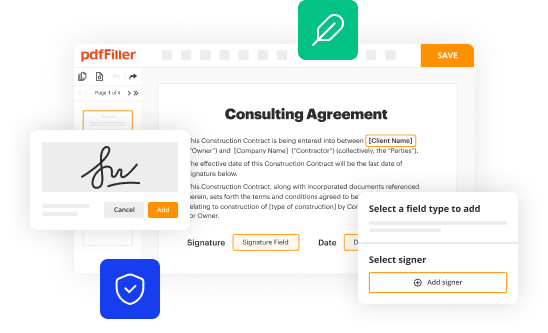
Editing history and physical template online
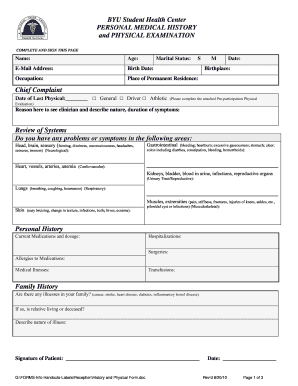
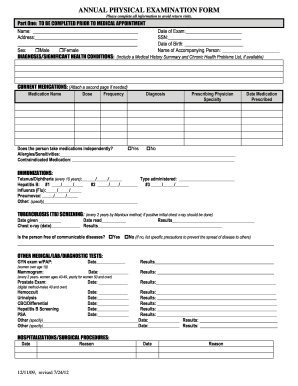
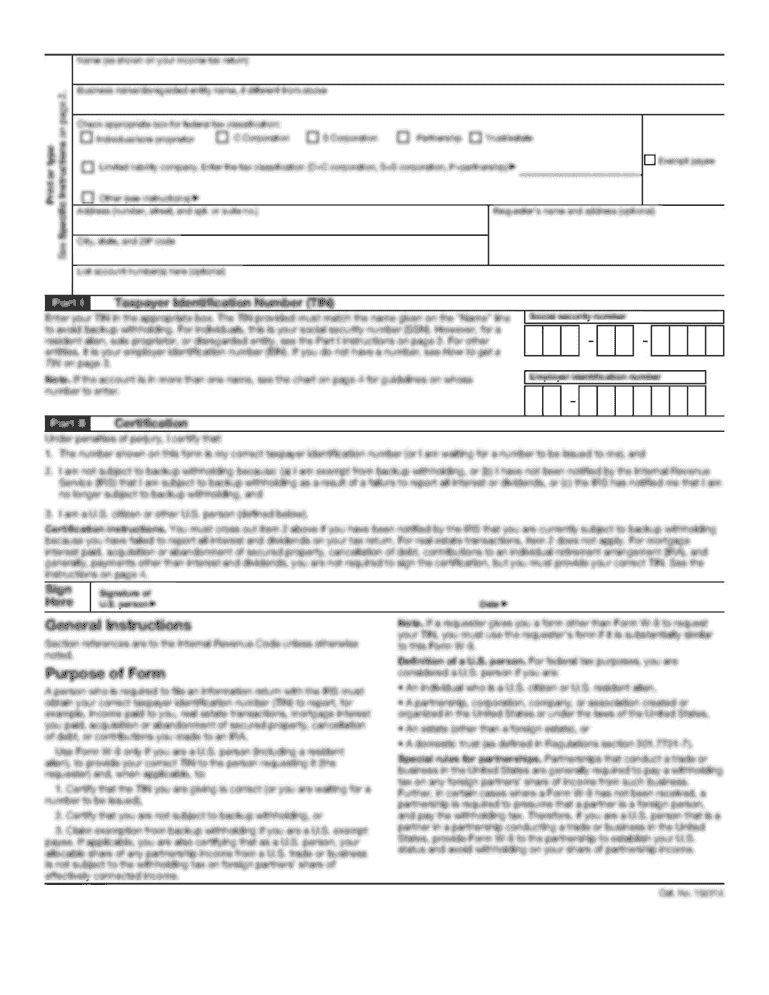
How to fill out history and physical template
Video instructions and help with filling out and completing history and physical template
Instructions and Help about clinical history physical form
Hello my name is Evan hotel I won the GP registrar's here, so I'm just going to find out a little about the problem that you've come in would that be all right oh yes I make some notes and basically this will just help me write it up on to the computer later on so just in your own words tell me what's brought you in today and well I've been getting some diarrhea raining yeah for the loss of Wow two three weeks mm-hmm okay so before two or three weeks no problems really um so before that no no I mean I know I have just been going normally which is once every couple of days or something yeah no no problems normally okay so just have a little more about the diarrhea what it's like and um so like what my Poona okay I'm tasks it's quite right it's funnier Jeff Lewis really normal I don't think there's any change in my color or anything um and I probably, but I'm just going a lot more often okay, so check do you have any blood in it at all oh um gosh yes I'm surprised haven't said that already isn't worrying me and yet that I've had em for a couple of days mm-hmm that is it difficult to flush away at all no no no it's not to have got to flush away yeah and do you ever see any food that's not digested properly in it hmm not no that wouldn't be something no yeah, so you said diarrhea but how many times a day does it actually happen um well I would say somewhere between well at the moment probably somewhere like yesterday was probably about eight times oh yeah um I don't think it's been like that every day for the last three weeks but up to eight times a day time yeah just get up at night to go to yeah yeah yeah never had to do that if you're losing sleep over it oh yeah yeah, and you have any tummy pain at all yes um yeah that's quite a sort of cramps and mainly just before I go to the restroom there can be other times but then does that pain go away once you've been to the toilet um yeah a little yeah I would say so a little mm-hmm does anything make the pain worse at all um just eating I do not like I can really think of any pointed your tummy exactly where is if it is it's just around the middle of really yeah and how do you describe that pain am I thought it's off so cramping I'm he is what he said isn't it yeah and how bad is it um can was excruciating and one was very little pain where would he put it is been they stopped I've had worse I'm sorry about for yeah, yeah so it's not agonized, but it certainly is there yeah okay, and you've told me about when it comes on and what makes it a little better and worse as well which is good I'm just going to ask the rest of the questions just about the whole gut itself give any gets go to chewing your food at all oh no no no mouth ulcers or anything like that um any difficulty swallowing your food at all do you ever get indigestion yeah not really ah sometimes maybe honor my going to weekend so good times okay but not usually okay, so this was only about three weeks ago that you've had lots okay and prior...
Fill history and physical : Try Risk Free
People Also Ask about history and physical template
Our user reviews speak for themselves
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Fill out your history and physical template online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.