Competency Assessment for POC Form: A Comprehensive Guide
Understanding the competency assessment for poc form
Competency assessments in Point of Care (POC) settings are crucial in ensuring that healthcare providers have the necessary skills and knowledge to deliver effective patient care. A competency assessment evaluates a healthcare professional’s abilities to perform specific tasks reliably and safely. It is a systematic approach that focuses on enhancing patient care quality and safety by ensuring that all staff are adequately trained and competent in their roles.
In clinical settings, Point of Care refers to the location where healthcare is provided, typically at the patient’s bedside, rather than in centralized lab facilities. This immediacy requires healthcare professionals to possess precise and up-to-date competencies to make decisions quickly and accurately. Therefore, implementing an efficient competency assessment for POC form not only reinforces best practices but also mitigates risks associated with medical errors.
Components of the competency assessment for poc form
A robust competency assessment for POC form includes several core components designed to evaluate various aspects of a healthcare professional’s capabilities. These components encompass knowledge, skill, and attitude assessments. Understanding these key elements is essential for anyone engaged in the POC framework.
This entails a theoretical evaluation, including quizzes and practical case studies, to ensure professionals understand essential medical concepts and protocols.
Essential clinical skills are evaluated through direct observation and practical demonstrations, ensuring that clinicians can perform required procedures effectively.
This focuses on professionalism, communication, and interaction with patients, which are critical for enhancing overall patient experience and care outcomes.
Effective scoring and evaluation criteria are critical in competency assessments. Objective metrics enable healthcare facilities to measure competence against established benchmarks, ensuring consistency and accountability within clinical care.
Step-by-step guide to completing the competency assessment for poc form
Filling out the competency assessment for POC form requires careful preparation and understanding of the roles involved. Prior to starting, gather all necessary documentation, including current certifications, training records, and any relevant clinical guidelines. Familiarizing yourself with your role and responsibilities is essential to accurately reflect your competencies.
Completing each section of the form systematically is vital for effectively documenting your capabilities.
Identify and document specific competency areas related to your role. Be precise in listing your experiences and qualifications.
Describe your skill competencies, citing specific protocols you’re adept at demonstrating. This can include giving examples of patient interactions.
Include how you acquire feedback from peers and supervisors, and discuss how you've utilized this feedback for improvement.
Accurate and honest reporting is paramount. Engage in self-assessment and reflection, identifying your areas of strength and opportunities for growth.
Leveraging interactive tools for enhanced assessment
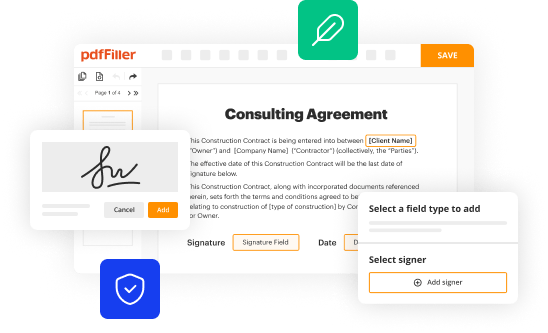
Digital solutions can simplify the management of competency assessments. Platforms like pdfFiller offer a variety of features, including editing and e-signing capabilities, making the form completion process smoother. The collaborative features enable team assessments, allowing multiple users to contribute and refine the document collectively.
Additionally, interactive learning tools such as case scenarios and simulations can significantly enhance skill practice. Utilizing ongoing education resources contributes to continuous professional development, ensuring healthcare providers stay updated on the latest practices and protocols.
Best practices for implementing competency assessments in poc settings
Establishing a regular assessment schedule is essential in maintaining competency. Whether monthly, quarterly, or annually, consistent evaluations ensure that skills and knowledge remain current and that the team is continuously improving.
Fostering a culture of continuous improvement encourages team members to participate in the assessment process actively. Open discussions about competency foster an environment of support and collective growth.
Regular assessments help ensure compliance with accreditation requirements, aligning with medical guidelines and enhancing patient care.
Having a systematic approach enables adjustments to be made based on performance, ensuring that all team members maintain the necessary competencies required for high-quality patient care.
Common challenges and solutions in competency assessment for poc
Implementing competency assessments can present challenges, including time constraints and resource limitations within healthcare settings. Additionally, some team members may resist initiatives perceived as critical.
Recognize potential barriers such as limited time and staffing challenges that might hinder effective assessments.
Utilize technology to streamline the assessment process. Consider engaging leadership to advocate for improved resources and staff support.
Developing a strategy to tackle these challenges is crucial for the success of competency assessments, reinforcing the value of ongoing training and assessment.
Tracking progress and outcomes
Monitoring competency levels over time is necessary for continual improvement. Effective documentation and record-keeping play a vital role in this process, allowing healthcare facilities to measure progress and address any skills gaps.
Employ data analysis methods to identify patterns in competency assessments, paving the way for targeted development opportunities.
Communicate results clearly to stakeholders, ensuring transparency about outcomes and areas requiring attention.
Tracking progress helps to maintain high standards of care and ensures that patients receive exemplary service from competent professionals.
Engaging with the pdfFiller platform for document management
pdfFiller offers an intuitive approach to editing and managing your competency assessment document. Features such as templates and editing tools make it easier to customize forms to meet specific assessment criteria.
Collaboration with peers using pdfFiller allows for real-time document management and feedback, facilitating a cooperative environment in which everyone contributes to the assessment process.
Using e-signatures and cloud storage provided by pdfFiller guarantees that all documents are securely stored and easily accessible.
The cloud-based nature of pdfFiller ensures that team members can access the competency assessment forms from any location, making the assessment process seamless.
Conclusion: The impact of competency assessment on quality care
Accurate competency assessments in POC environments are fundamentally linked to improved patient care. A structured approach ensures that healthcare professionals are capable and up-to-date with necessary skills, directly correlating to enhanced patient outcomes.
As healthcare continues to evolve, so too will the methodologies behind competency assessments. Staying ahead of trends and committing to continuous learning will define the future of competency assessments, ensuring that patients always obtain the highest level of care possible.