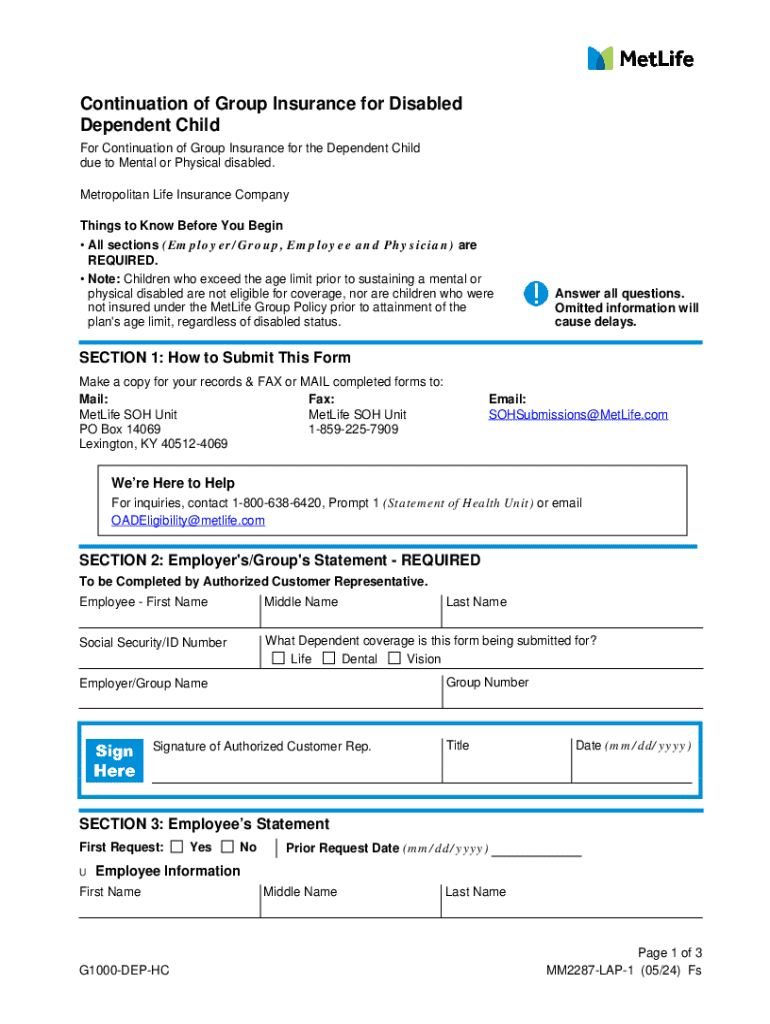
Get the free Continuation of Group Insurance for Disabled Dependent Child
Get, Create, Make and Sign continuation of group insurance
Editing continuation of group insurance online
Uncompromising security for your PDF editing and eSignature needs
How to fill out continuation of group insurance
How to fill out continuation of group insurance
Who needs continuation of group insurance?
Continuation of group insurance form: A comprehensive guide
Understanding the continuation of group insurance
Continuation of group insurance allows individuals to maintain access to their health and financial benefits after key life changes such as job loss or retirement. This safety net is crucial, as disruptions in health coverage can severely impact individuals and their families, both financially and health-wise. Group insurance plans often provide more comprehensive benefits at lower costs compared to individual plans, making it essential for eligible individuals to navigate the continuation process effectively.
The benefits associated with group insurance plans typically include lower premiums, larger networks of providers, and comprehensive coverage options. Understanding these advantages sets the stage for appreciating why continuation should be prioritized when experiencing transitions that may affect one's insurance status.
Eligibility criteria
To qualify for continuation of group insurance, certain eligibility criteria must be met. Individuals usually qualify if they are leaving employment, whether due to termination, retirement, or a reduction in hour worked that affects coverage. Key scenarios include losing a job or transitioning into retirement, both of which can open the door for continuation options under specific regulations.
How to initiate the continuation process
Initiating the continuation process of group insurance is relatively straightforward but requires careful attention to detail. The first step is to identify your insurance provider to ensure you have the correct forms and contact information. Each provider may have different requirements and timelines, so understanding these can simplify the process significantly.
Next, gather the necessary documentation. This often includes proof of employment termination or retirement, such as a termination letter or retirement notice. Completing the continuation form accurately is crucial for a smooth transition. It's important to take your time to ensure all necessary details are included before submission.
Common mistakes to avoid
As with any administrative process, there are common pitfalls to be wary of when requesting the continuation of group insurance. One significant mistake is failing to submit documents on time. Most insurance policies will have strict deadlines that must be adhered to, so be mindful of these timelines.
Another mistake is not fully understanding your coverage options. Taking the time to understand what is available and any potential costs or changes will lead to better decision-making during this transitional period.
COBRA continuation coverage explained
The Consolidated Omnibus Budget Reconciliation Act (COBRA) is a significant regulation enabling eligible employees to continue their group health insurance after leaving employment. COBRA benefits allow individuals to maintain the same coverage they had while employed, but often at a higher premium since the employer subsidy is no longer available. Understanding COBRA is crucial for anyone considering health insurance continuation options.
Eligibility for COBRA coverage typically applies to employees of companies with 20 or more employees and includes events like job loss, reduced hours, or significant life changes such as divorce. It's essential to remember that COBRA coverage is a temporary solution, not a permanent replacement for group insurance.
How to apply for COBRA continuation coverage
Applying for COBRA continuation coverage involves several clear steps. First, you should receive a notice from your employer detailing your rights under COBRA. If this does not occur, initiate contact with your HR department to inquire about eligibility. Once confirmed, you will then need to complete a COBRA application form, typically provided by your employer or health plan.
Each state may have different deadlines for applying for COBRA coverage—typically, you have 60 days to apply after you lose your group insurance. Furthermore, there may be grace periods for premium payments, so it’s important to keep track of these dates to avoid accidental lapses in coverage.
Coverage options and limitations
When considering the continuation of group insurance, various coverage options become available. Typically, these options can include health insurance, dental plans, vision care, and even life insurance under certain group policies. Each of these coverage types will have specific details on what is included or excluded, and understanding these nuances is essential for making informed decisions.
Coverage duration can vary significantly. Under COBRA, for instance, continuation coverage usually lasts for 18 months but may extend to 36 months depending on qualifying events. Factors such as job loss, divorce, or the passing of the insured can influence how long coverage remains effective.
Managing your group insurance continuation
Once you've initiated the continuation of group insurance, managing that coverage requires remaining informed about key aspects. A frequently asked question pertains to how long one can remain on their former employer’s plan, which typically ranges from 18 to 36 months, depending on the specific circumstances. However, it's essential to regularly verify any specific policy provisions, as these details can vary.
Additionally, understanding what happens if you miss a premium payment is crucial. Most insurance policies provide a grace period, but failing to make timely payments could result in loss of coverage. Keeping track of all premium due dates is imperative to avoid such pitfalls.
Contacting customer support
Effective communication with your insurance provider plays a vital role in ensuring a seamless experience. When reaching out, it’s beneficial to have your policy number, personal information, and any relevant documents at hand to expedite the process. This preparation allows for a more focused conversation, ultimately leading to clearer answers to pressing questions.
Insurance representatives can provide valuable insight into your specific coverage terms, options for premium payments, and available assistance programs. Don’t hesitate to ask questions if you’re not clear about something; your understanding is essential for effective management of your continuation options.
Resources for assistance
While navigating the continuation of group insurance form can feel daunting, several resources can ease the process. Online tools and calculators can provide personalized assessments of your insurance needs, helping you decide whether continuation is the right choice for you. These resources are often available through employment offices and insurance provider websites.
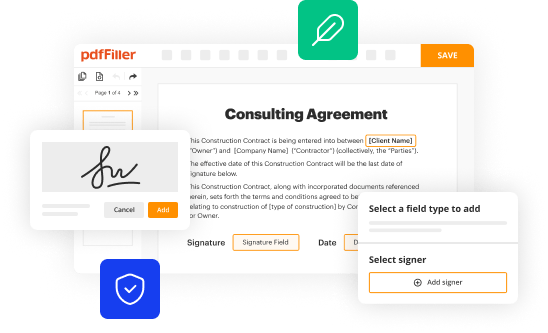
Additionally, utilizing document management features on pdfFiller can streamline the process of filling out, signing, and managing forms related to continuation of group insurance. This platform allows users to store and organize their insurance documents in one secure location, eliminating the hassle of misplaced paperwork.
Navigating the transition period
Transitioning from employer-sponsored coverage to continuation plans can be challenging but manageable with the right strategies. Understanding your new options, such as individual plans or marketplace options, is key. These may be more cost-effective or provide better health options depending on your health situation and financial circumstances.
Moreover, it's essential to anticipate potential gaps in coverage and develop a plan to avoid them. This could mean coordinating the start of a new insurance plan with the termination of the previous one or finding temporary coverage while transitioning. Communicating these changes to family members is also critical to ensure dependent coverage is managed appropriately.
Long-term considerations
As you explore the continuation of group insurance, it's also essential to think about future coverage options once your continuation period ends. Transitioning to individual plans might be necessary and evaluating your long-term insurance needs is beneficial. Assessing factors such as family health history and potential medical expenses will guide your decisions regarding future coverage.
Additionally, maintaining proper records for future reference is vital. Keeping documentation organized enhances your ability to navigate any future claims efficiently and ensures all information is readily available should you need it. Tools like pdfFiller can assist in record-keeping, making it straightforward to manage and store insurance documentation securely.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete continuation of group insurance online?
How do I make edits in continuation of group insurance without leaving Chrome?
How do I edit continuation of group insurance on an iOS device?
What is continuation of group insurance?
Who is required to file continuation of group insurance?
How to fill out continuation of group insurance?
What is the purpose of continuation of group insurance?
What information must be reported on continuation of group insurance?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.