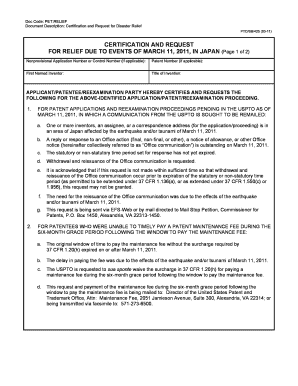
Get the free Cvs Caremark Prior Authorization Form
Get, Create, Make and Sign cvs caremark prior authorization
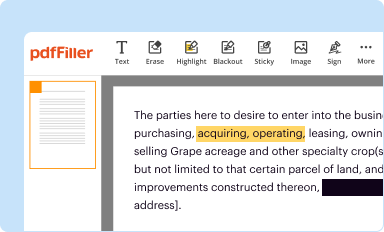
Editing cvs caremark prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cvs caremark prior authorization
How to fill out cvs caremark prior authorization
Who needs cvs caremark prior authorization?
Understanding the CVS Caremark Prior Authorization Form
Understanding prior authorization: What it is and why it matters
Prior authorization is a critical process employed by health insurance companies to control costs and ensure that patients receive appropriate care. This mechanism requires healthcare providers to obtain approval from the insurance company before delivering specific treatments or medications. It's pivotal for safeguarding against unnecessary treatments and managing healthcare spending.
For both patients and healthcare providers, this process significantly impacts treatment timelines and healthcare decisions. Understanding this can ease frustrations when patients experience delays in receiving prescribed medications or services. CVS Caremark serves a vital role by being a key player in the prior authorization landscape, conducting reviews to ensure that medication and service requests are justified.
What is the CVS Caremark prior authorization form?
The CVS Caremark prior authorization form functions primarily as a request mechanism. It provides a structured format for healthcare providers to communicate the necessity of specific medications or services that require approval before coverage can be granted. This ensures that both patients and providers navigate the complexities of insurance policies effectively.
Certain types of medications and services, especially those that are high-cost or involve specialized treatments, typically require prior authorization. This can include specialty medications, certain imaging services, or surgeries. The form is designed to capture detailed information regarding the requested treatment, the patient's medical history, and the rationale for the request.
How to obtain the CVS Caremark prior authorization form
Accessing the CVS Caremark prior authorization form is straightforward. The primary source is the official CVS Caremark website, where users can find downloadable versions of the form. Simply visit the site, navigate to the prescription details or prior authorization section, and access the form directly.
Once located, you can download and save the form for your convenience. It's also beneficial to ensure that you are using the most up-to-date version available to avoid any potential issues with outdated information. Alternatively, your healthcare provider can also help you obtain this form if needed.
Step-by-step guide to completing the CVS Caremark prior authorization form
Filling out the CVS Caremark prior authorization form correctly is crucial for its approval. Below is a step-by-step guide to ensure all necessary information is captured:
Common mistakes to avoid when filling out the form
Filling out the CVS Caremark prior authorization form can be time-consuming, and various pitfalls can lead to delays in approval. Here are some common mistakes to avoid:
Submitting the CVS Caremark prior authorization form
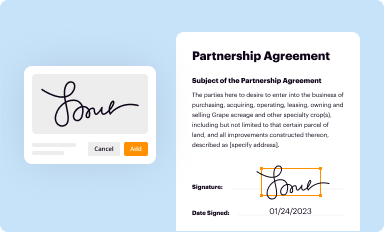
After completing the form, the next step is submission. There are various methods available for sending it to CVS Caremark, including fax, email, and online portal submissions. Each method has different requirements, so it’s essential to choose the one that best aligns with your preferences.
Once submitted, confirming the receipt of your submission is crucial, as this can provide peace of mind and assurance that your request is being processed. It's also beneficial to ask about the expected timeline for approval to manage expectations while waiting.
What happens after submission?
After the CVS Caremark prior authorization form is submitted, it enters a review process. This process typically involves evaluating the necessity of the requested medication or service based on the information provided. Patients and healthcare providers should stay informed about what to expect.
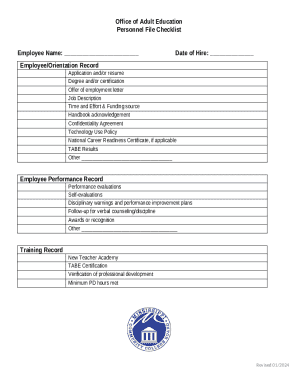
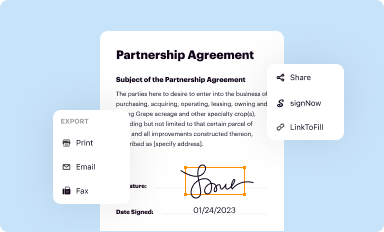
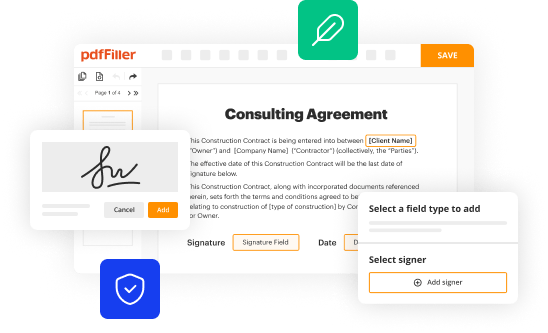
Key resources available through pdfFiller
pdfFiller offers a suite of features for users managing the CVS Caremark prior authorization form. An editable PDF format means users can fill out the form at their convenience and save it without error. Additionally, the eSignature capability expedites processing times, allowing users to sign documents quickly and easily.
Collaboration is seamless through pdfFiller as multiple healthcare team members can work together on document management. Cloud-based storage ensures that all documents are readily accessible and can be managed efficiently, allowing for ongoing updates or revisions as necessary.
Troubleshooting common issues with prior authorization
Experiencing delays or denials in prior authorization requests can be frustrating. It's essential to understand common issues and potential solutions. Delays often stem from incomplete submissions or failures to meet specific criteria set by the health insurance provider.
If a request is denied, consider the reasons—many times, denials occur due to missing supporting documentation. Understanding these reasons empowers patients and providers to address issues proactively. If the situation becomes muddled, do not hesitate to contact customer support for assistance, as they can often provide clarifications and next steps.
Tips for a smoother prior authorization experience
Navigating the prior authorization process can be daunting, but certain best practices can ease the experience. Maintaining clear documentation is vital; regularly update records and retain copies of forms submitted. Close coordination with your healthcare provider also ensures that all necessary information is communicated effectively.
Consider setting reminders for submission dates and renewals to avoid lapses in authorization. This proactive approach not only prevents delays but also allows timely adjustments to healthcare plans as needed.
How pdfFiller enhances your document handling experience
pdfFiller stands out as a premier solution for document handling, especially when it comes to navigating healthcare forms. Unique features include the ability to seamlessly edit PDFs, which empowers users to make necessary adjustments quickly. The cloud-based platform simplifies document management, making access and storage both efficient and reliable.
Utilizing a platform like pdfFiller not only streamlines the prior authorization process but also enhances overall productivity by centralizing document management. This can be especially beneficial for healthcare teams working collaboratively to manage patient needs and paperwork efficiently.
User testimonials: Success stories with CVS Caremark and pdfFiller
Many users have shared stories about how the CVS Caremark prior authorization process, when coupled with pdfFiller's capabilities, resulted in smoother experiences. Patients often appreciate how quickly they can submit requests and track their approvals, reducing anxiety over medication access.
Healthcare teams also benefit from the collaboration tools that pdfFiller provides, which allow multiple stakeholders to manage documents simultaneously, leading to fewer missed communications and expedited approvals. These success stories highlight the tangible benefits of integrating robust document management solutions in navigating the healthcare landscape.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit cvs caremark prior authorization on a smartphone?
How do I fill out the cvs caremark prior authorization form on my smartphone?
How can I fill out cvs caremark prior authorization on an iOS device?
What is cvs caremark prior authorization?
Who is required to file cvs caremark prior authorization?
How to fill out cvs caremark prior authorization?
What is the purpose of cvs caremark prior authorization?
What information must be reported on cvs caremark prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.