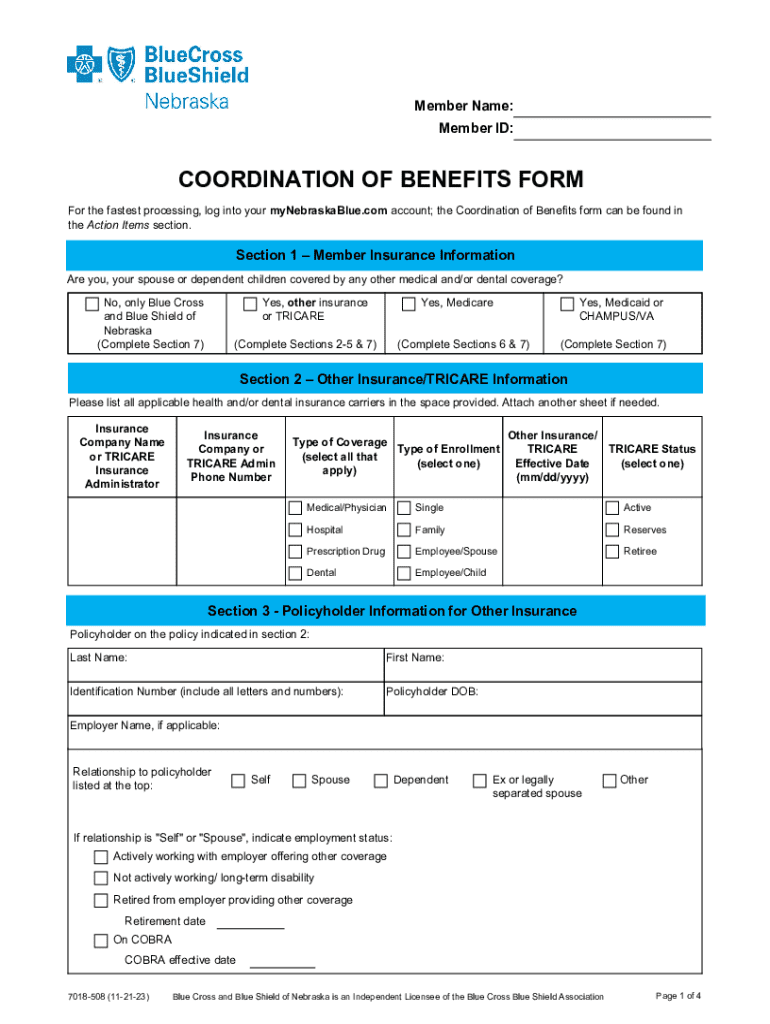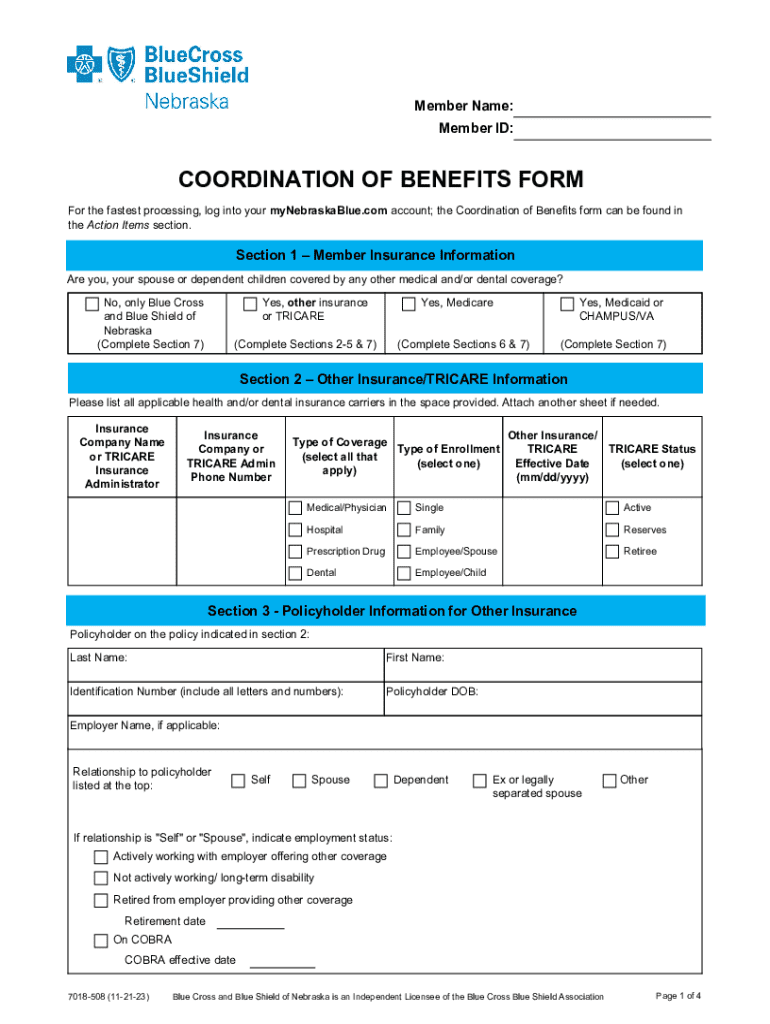
Get the free Coordination of Benefits Form
Get, Create, Make and Sign coordination of benefits form
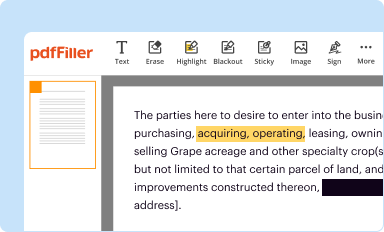
Editing coordination of benefits form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out coordination of benefits form
How to fill out coordination of benefits form
Who needs coordination of benefits form?
Coordination of Benefits Form: A How-to Guide
Understanding the Coordination of Benefits Form
The Coordination of Benefits (COB) form is a vital document in the healthcare industry, specifically designed for individuals covered by more than one health insurance policy. Its primary aim is to ensure that the right amount of reimbursement is applied when an individual files a claim. It effectively helps streamline healthcare transactions and reduces the chances of errors when determining which insurance provider is responsible for a particular service.
Filling out the COB form accurately is crucial, as it influences the process of claim processing and payment decisions. If discrepancies arise due to incorrect information, patients may face delays in reimbursements, or even worse, denial of claims altogether, leading to financial strain.
Who needs to fill out the Coordination of Benefits Form?
The Coordination of Benefits form is necessary for a variety of individuals and contexts. Primarily, anyone with multiple health insurance coverages should complete it. This includes:
Understanding who needs to complete this form can greatly simplify billing and ensure that patients receive the maximum benefits available to them.
Key components of the Coordination of Benefits Form
The Coordination of Benefits form contains several critical components that must be filled out correctly to facilitate the processing of insurance claims. Some of these key components include:
Each part of the form is interlinked to ensure a seamless claim verification process between insurers.
Step-by-step instructions for filling out the Coordination of Benefits Form
Filling out the Coordination of Benefits form can seem daunting, but following a methodical approach can streamline the process. Here’s a step-by-step guide to ensure you complete it accurately:
By adhering to these steps, you can minimize errors and ensure your claims are processed promptly and efficiently.
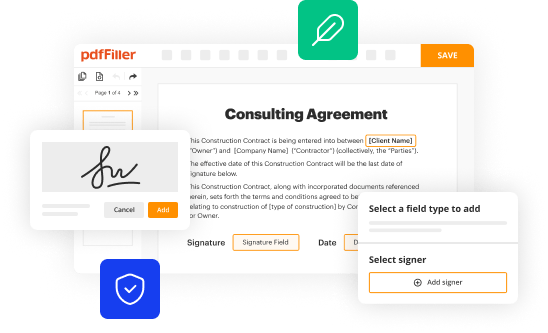
Editing and customizing your Coordination of Benefits form
Editing the Coordination of Benefits form is crucial for adapting to your specific insurance needs. Using tools like pdfFiller allows users to modify text, add fields, and insert images easily. This functionality can be particularly beneficial when dealing with multiple insurance providers, as you may need to reuse the form for different claims periodically.
The benefits of digital editing over traditional print forms are significant. For one, digital forms can be updated and saved efficiently, reducing the chances of error. Additionally, having a cloud-based editing platform means users can access their forms from anywhere, making the process more efficient, especially for busy individuals juggling multiple policies.
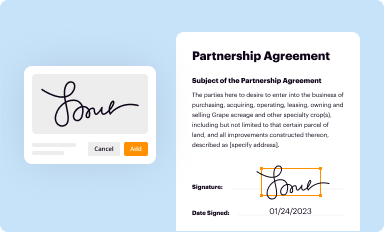
Signing the Coordination of Benefits Form
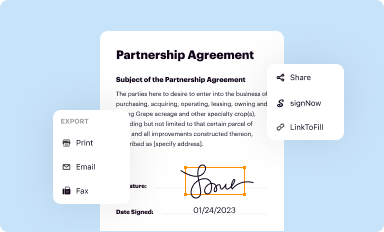
A signature on the Coordination of Benefits form is essential to authorize the processing of claims with multiple insurers. pdfFiller offers efficient eSigning options that are secure and user-friendly, allowing you to electronically sign the document right after completing it.
To eSign, simply follow the prompts to create your electronic signature and affix it to the document. This step will help expedite the claims process, as most insurers prioritize claims with valid signatures and completed forms.
Submitting the Coordination of Benefits Form
The submission process for your Coordination of Benefits form is crucial and can vary based on your insurance provider's requirements. Typically, forms can be submitted in several ways, including by mail, online, or in person.
To ensure your submission is efficient, double-check that all information is accurately completed, and consider making copies for your records. Keeping track of your submission date can also help when following up on claims.
Common mistakes to avoid when filling out the Coordination of Benefits Form
When it comes to filling out the Coordination of Benefits form, attention to detail is essential. Several common mistakes can lead to issues in processing.
Being aware of these pitfalls enables you to approach the COB form with greater confidence and efficacy.
Frequently asked questions about the Coordination of Benefits Form
Many individuals have queries regarding the COB form process. Understanding common questions can clarify the path ahead.
Being informed about these aspects can enhance your ability to navigate the health insurance landscape effectively.
Troubleshooting issues with the Coordination of Benefits Form
If you encounter issues stemming from the Coordination of Benefits form, there are essential steps you can take to troubleshoot effectively. First, review the completed form to ensure all information is correct and current.
Following these steps will help you effectively manage any setbacks and ensure that you receive the benefits you are entitled to.
Benefits of using pdfFiller for your Coordination of Benefits Form
Choosing pdfFiller for managing your Coordination of Benefits form offers numerous advantages. The platform provides seamless cloud-based access, allowing users to edit the COB form from any device, anywhere. This ease of access is particularly beneficial for individuals involved in managing multiple insurance claims, as it centralizes important documentation.
Moreover, pdfFiller boasts collaborative features that are invaluable for teams managing health insurance claims. These tools facilitate clear communication and operational efficiency by allowing team members to work simultaneously on documents to reduce errors. Enhanced security measures protect personal data, ensuring peace of mind during the claims process.
Staying organized with multiple insurance plans
Managing several insurance documents can be overwhelming. However, employing systematic strategies can significantly alleviate the stress associated with juggling multiple plans. Consider utilizing pdfFiller for storing and organizing your health insurance files in one accessible location.
Setting reminders for regular updates to your Coordination of Benefits form is also a proactive approach. Keeping documents current minimizes the risk of errors during the claims process, ensuring you maintain adequate coverage across various policies.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my coordination of benefits form in Gmail?
How do I fill out the coordination of benefits form form on my smartphone?
How do I edit coordination of benefits form on an Android device?
What is coordination of benefits form?
Who is required to file coordination of benefits form?
How to fill out coordination of benefits form?
What is the purpose of coordination of benefits form?
What information must be reported on coordination of benefits form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.