Get the free Cervical Cancer Prior Authorization Request
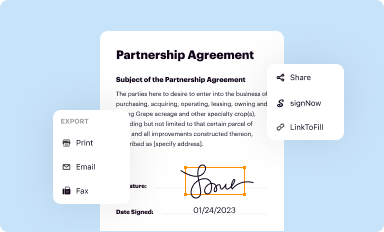
Get, Create, Make and Sign cervical cancer prior authorization
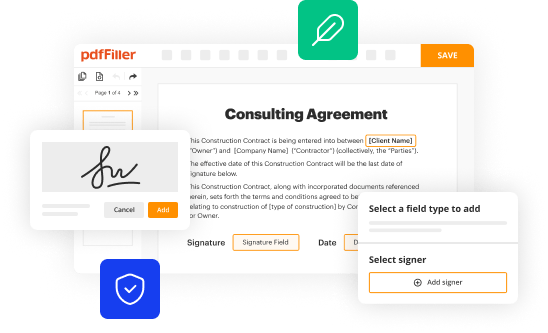
Editing cervical cancer prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cervical cancer prior authorization
How to fill out cervical cancer prior authorization
Who needs cervical cancer prior authorization?
Cervical Cancer Prior Authorization Form: A Comprehensive Guide
Understanding the cervical cancer prior authorization process
Prior authorization is a crucial step in the healthcare process, particularly when it comes to treatments for cervical cancer. This process involves obtaining approval from an insurance provider before a specific treatment can be rendered. Without this authorization, patients may face significant out-of-pocket costs or find that their treatment is not covered at all. In the context of cervical cancer, where timely and appropriate treatment is often essential, the prior authorization process plays a fundamental role in facilitating access to necessary therapies.
The importance of prior authorization in cervical cancer treatment cannot be overstated. It ensures that the proposed treatment aligns with evidence-based guidelines and meets the standards of medical necessity as defined by insurance companies. Understanding insurance requirements is a vital aspect of the prior authorization process because each provider may have different criteria that must be met for approval.
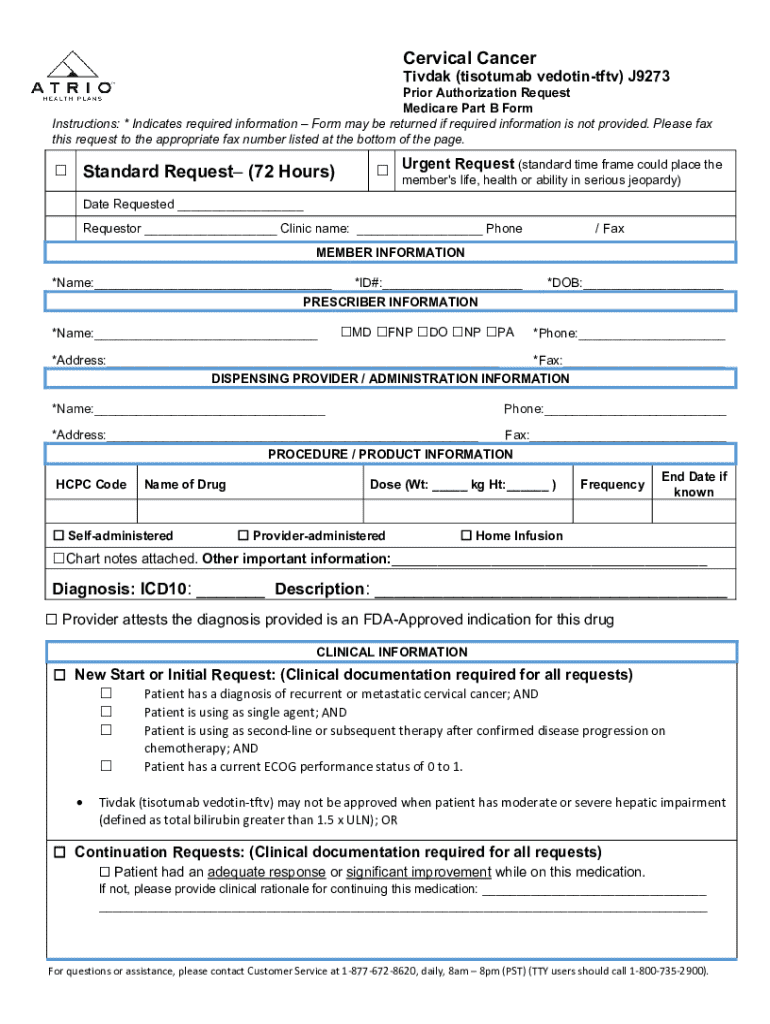
Key components of the cervical cancer prior authorization form
The cervical cancer prior authorization form is designed to capture essential information that allows insurers to assess the appropriateness of the requested treatment. Each section of the form serves a distinct purpose, which helps streamline the approval process. Here are some key components that should be clearly outlined on the form:
Step-by-step guide to filling out the cervical cancer prior authorization form
Filling out the cervical cancer prior authorization form can seem daunting but following a structured approach can simplify the process. Here’s a detailed step-by-step guide:
Tools for managing your form submission
Using efficient tools can greatly enhance the process of managing your cervical cancer prior authorization form. pdfFiller is an excellent solution for anyone needing a comprehensive document management system. It supports effective editing, eSignature, and team collaboration, simplifying the often-complex submission process.
Common pitfalls to avoid when submitting the form
Successfully submitting your cervical cancer prior authorization form hinges on attention to detail. There are common pitfalls that applicants should be aware of to maximize the chances of approval.
Tracking the status of your prior authorization request
After submitting your cervical cancer prior authorization form, understanding how to track its status is essential. Effective follow-up can make a significant difference in expediting care.
Printable resources and templates
Utilizing printable resources and templates can further streamline the process of submitting a cervical cancer prior authorization form. pdfFiller offers a range of templates designed to meet specific needs.
Interactive tools to enhance your experience
Engaging with interactive tools can elevate the experience of navigating the cervical cancer prior authorization process. These resources provide valuable insights and support.
Legal considerations regarding prior authorization forms
It's essential to be aware of the legal aspects surrounding the cervical cancer prior authorization form. Knowledge of patient rights and ethical handling of documents can help navigate potential pitfalls.
Enhancing your document management strategy
Implementing a robust document management strategy is vital, particularly when dealing with medical forms like the cervical cancer prior authorization form. A cloud-based solution like pdfFiller can vastly improve organization and accessibility.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an electronic signature for the cervical cancer prior authorization in Chrome?
How do I edit cervical cancer prior authorization straight from my smartphone?
How do I complete cervical cancer prior authorization on an iOS device?
What is cervical cancer prior authorization?
Who is required to file cervical cancer prior authorization?
How to fill out cervical cancer prior authorization?
What is the purpose of cervical cancer prior authorization?
What information must be reported on cervical cancer prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.