Get the free Cda-amc Reimbursement Review
Get, Create, Make and Sign cda-amc reimbursement review
How to edit cda-amc reimbursement review online
Uncompromising security for your PDF editing and eSignature needs
How to fill out cda-amc reimbursement review
How to fill out cda-amc reimbursement review
Who needs cda-amc reimbursement review?
Comprehensive Guide to the CDA-AMC Reimbursement Review Form
Overview of CDA-AMC Reimbursement Review Form
The CDA-AMC reimbursement review form is a critical document in the healthcare reimbursement process, designed to assess claims and ensure that costs incurred meet predefined standards. Its primary purpose is to streamline reimbursement evaluations, ultimately aiding in budgeting and resource allocation within healthcare organizations. The importance of the CDA-AMC review process cannot be overstated; it directly impacts the financial health of healthcare providers, including clinics, hospitals, and individual practitioners, while affecting patients through their access to necessary services.
Decisions made regarding reimbursements influence a wide range of stakeholders, from healthcare providers who rely on prompt payments for their services to patients who may be responsible for various out-of-pocket expenses. Understanding the nuances of the CDA-AMC reimbursement review form is essential for anyone involved in healthcare management and finance.
Understanding the CDA-AMC Process
The CDA-AMC system, which stands for Claims Documentation and Analytics Management Corporation, is a mechanism that helps streamline the review of reimbursement claims submitted by healthcare entities. The system facilitates efficient communication among stakeholders, including payers, providers, and regulatory agencies. The key stakeholders involved in this process span a wide range, encompassing healthcare providers who submit claims, insurance companies that review them, and government entities that regulate reimbursement practices.
Typically, the CDA-AMC review process can be broken down into several stages: initial submission, primary evaluation, and final decision-making. Each stage has set timelines to ensure that claims are processed efficiently, allowing stakeholders to predict outcomes and manage their finances more effectively. Understanding these timelines is crucial for anyone looking to navigate the reimbursement landscape successfully.
Step-by-step guide to completing the CDA-AMC reimbursement review form
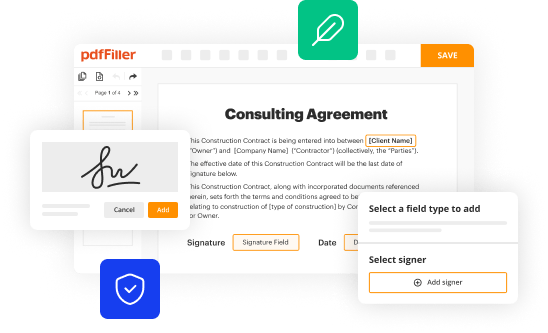
Completing the CDA-AMC reimbursement review form can seem daunting at first, but following a structured approach can simplify the process. The first step involves accessing the form itself. You can find it on pdfFiller, a platform known for document management solutions. To navigate pdfFiller effectively, familiarize yourself with the site layout, focusing on the search functions and categories available for healthcare-related forms.
Once you have located the form, filling it out accurately is the next crucial step. Each section of the form requires specific information, such as patient details, services rendered, and financial data. Providing precise information is paramount because any discrepancies can lead to denial or delays in reimbursement. A common pitfall is rushing through the form; read instructions carefully to avoid easily avoidable mistakes.
Next is uploading supporting documents; most submissions require specific documentation to substantiate the claims made within the review form. Ensure that you include all necessary documents as outlined in the submission guidelines. Uploading these documents on pdfFiller is straightforward—simply follow the upload prompts and check for file type compliance to avoid rejection due to format issues.
Before finalizing your submission, take the time to review and edit your submission on pdfFiller, utilizing its editing tools for any last-minute adjustments or corrections. This practice helps ensure that everything is accurate and compliant with requirements, significantly reducing the risk of denial.
Electronic signing of the CDA-AMC reimbursement review form
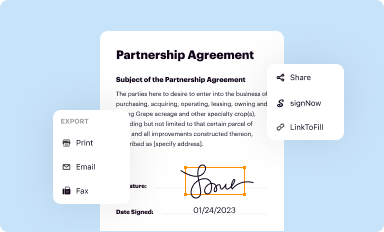
In the realm of healthcare documentation, electronic signing has emerged as a vital step in the reimbursement process. Employing pdfFiller’s eSigning feature not only enhances efficiency but also adds a layer of security to your submissions. Electronic signatures are legally recognized and provide assurance that the document has not been altered post-signature.
Using pdfFiller’s eSigning function is intuitive; upon completion of the form, you'll have the option to sign digitally. The platform employs robust security measures to protect the integrity of signatures, ensuring that sensitive information is safeguarded throughout the reimbursement process. Familiarizing yourself with this feature can expedite your documentation workflow significantly.
Submitting your form
Once you've completed and electronically signed the CDA-AMC review form, the next step is submission. pdfFiller allows users to submit their forms directly from the platform, simplifying the entire process. Simply click the submit button and follow any additional prompts provided by the platform to finalize your submission.
Tracking the status of your submission is also a critical component of the process. Make use of any tracking features pdfFiller provides to stay informed about the status of your claim—including any updates or requirements for follow-up actions. After submission, you should anticipate a time frame for responses, allowing you to plan ahead for any additional needs your organization might encounter.
FAQs regarding the CDA-AMC reimbursement review process
Navigating the CDA-AMC reimbursement review process can present challenges, so it's valuable to know some frequently asked questions related to it. Many clients inquire whether electronic submissions are accepted in all jurisdictions, answers vary, but most do allow for electronic processing due to its efficiency. Others might wonder about the possibility of appeal if a claim is denied. Generally, there is a formal procedure for appeals, and understanding this process can help in preparing for potential setbacks.
If you encounter issues during the submission, direct assistance is available through pdfFiller's support team, making it easier for users to resolve concerns specific to the platform and reimbursement process. Accessing resources and guidance offered by pdfFiller can significantly enhance your understanding and ability to navigate the complexities involved.
Benefits of using pdfFiller for CDA-AMC documentation
pdfFiller offers numerous advantages for managing CDA-AMC documentation, enabling users to access forms and templates from virtually anywhere. Its cloud-based structure means both individuals and teams can collaborate seamlessly on document preparation and submission processes. The platform also supports easy sharing, real-time edits, and compliance checks that streamline workflows for healthcare providers and administrative staff alike.
Moreover, the user-friendly interface reduces the learning curve for new users. Enhanced features such as templates specifically designed for healthcare claims can save time and reduce frustration. Embracing pdfFiller not only improves documentation efforts but also fortifies an organization’s workflow, enhancing financial outcomes in the long run.
Troubleshooting common issues
As with any digital platform, users may encounter some technical issues while filling out or submitting the CDA-AMC reimbursement review form. Common challenges may include difficulties in uploading documents due to format errors or issues with the eSignature process not completing. To address these, first ensure your files meet the required specifications—pdfFiller's guidelines should provide clarity on acceptable formats.
Should issues persist, reaching out to pdfFiller support can be a straightforward solution. The support team is equipped to handle inquiries, offering direct assistance tailored to your specific needs, thereby enhancing your experience with the platform. Staying proactive in troubleshooting ensures that your claims are submitted timely and efficiently.
Testimonials and success stories
The impact of the CDA-AMC reimbursement review form is often highlighted through firsthand accounts from users who have successfully navigated the process. Healthcare professionals frequently share success stories about how they streamlined their claim submissions and resolved reports of denied claims rapidly due to utilizing pdfFiller's efficient platform.
Feedback emphasizes the value of having a centralized tool for all documentation needs, praised for enhancing productivity and ensuring timely reimbursements. These testimonials reinforce the effectiveness of using pdfFiller for managing the entire reimbursement process, illustrating how the platform helps to alleviate many challenges faced in healthcare documentation.
Next steps for users after submission
After submitting the CDA-AMC reimbursement review form, it's essential to know your next steps. This typically involves monitoring the submission status through pdfFiller’s tracking features, as this will provide insight into whether your claim is being processed or has been flagged for additional review. Familiarizing yourself with expected response timelines can help manage expectations and inform your financial planning.
Users should also be prepared for possible follow-up actions, such as providing additional documentation or appealing a denial if necessary. Understanding these avenues not only fortifies your position during the review process but also equips you with the tools needed to respond proactively, fostering better outcomes for your claims in the long term.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I modify cda-amc reimbursement review without leaving Google Drive?
How do I complete cda-amc reimbursement review online?
How do I fill out cda-amc reimbursement review on an Android device?
What is cda-amc reimbursement review?
Who is required to file cda-amc reimbursement review?
How to fill out cda-amc reimbursement review?
What is the purpose of cda-amc reimbursement review?
What information must be reported on cda-amc reimbursement review?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.