Get the free Consent to Treatment and Recipient’s Rights
Get, Create, Make and Sign consent to treatment and
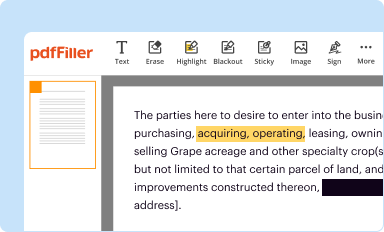
Editing consent to treatment and online
Uncompromising security for your PDF editing and eSignature needs
How to fill out consent to treatment and
How to fill out consent to treatment and
Who needs consent to treatment and?
Consent to treatment and form: A comprehensive guide
Understanding consent to treatment
Consent to treatment is a foundational principle in healthcare, representing an agreement between a patient and healthcare provider before any medical intervention. This consent empowers patients, giving them a say in their own health decisions, and fosters trust in the doctor-patient relationship. Medical procedures, whether diagnostic or therapeutic, must be accompanied by clear patient consent, as any treatment provided without it may lead to ethical and legal repercussions.
The importance of obtaining patient consent cannot be overstated. It not only respects the autonomy of the patient but also aligns with legal and professional standards. Without proper consent, healthcare providers risk legal liabilities, including malpractice suits. Thus, understanding the nature of consent is crucial for both patients and providers, as it establishes the groundwork for a respectful, informative, and collaborative healthcare experience.
Legal implications
Legally, consent to treatment must adhere to specific requirements to be considered valid. Regulations often stipulate that patients should be mentally competent, meaning they must understand the implications of their decisions. Furthermore, consent must be given voluntarily, without coercion or undue pressure. Failure to secure proper consent can lead to significant legal consequences, such as charges of battery or negligence. In some healthcare jurisdictions, medical professionals may even face disciplinary action from licensing boards for noncompliance.
Consequently, understanding these legal implications is important for healthcare providers to ensure they’re operating within lawful parameters. Continuous education on consent laws specific to their locale helps protect not only their patients but also their professional standing.
Types of consent
Various forms of consent exist within the realm of healthcare, primarily categorized into informed consent, implied consent, and written consent. Each form serves a different purpose and is applicable in specific scenarios.
Informed consent
Informed consent is the most critical type involved in medical practice. It requires healthcare providers to give patients detailed information about the treatment’s risks, benefits, and alternatives, thus enabling patients to make educated decisions regarding their health. The three key components of informed consent are information disclosure, patient understanding, and voluntariness. Without proper adherence to these elements, the consent cannot be deemed valid, potentially exposing providers to risks of malpractice.
Implied consent
Implied consent occurs in situations where a patient’s consent is assumed based on their actions or the circumstances, often seen in emergency situations. For example, if a patient is unconscious and requires immediate medical care, medical professionals are empowered to act fast without explicit consent, given the situation’s urgency.
Written consent
Written consent becomes significant when a formal documentation process is necessary. Medical procedures involving potential risks often require patients to sign a consent form documenting their understanding and agreement to the proposed interventions. Such instances commonly include surgeries, invasive tests, or treatments with substantial side effects. Written consent ensures both parties are clear about the patient’s choices and helps protect the healthcare facility from potential litigation.
The role of consent forms
Consent forms play an essential role in documenting a patient’s agreement to treatment. They act as a formal record of the consent process and are crucial in enhancing transparency between patients and healthcare providers. By providing written proof, these forms serve as a protective measure for both parties, ensuring that all discussions regarding the treatment have been adequately captured.
A well-structured consent form typically includes several components. Essential items such as patient details, a thorough explanation of the proposed treatment, associated risks, anticipated benefits, and both patient and provider signatures form the backbone of these documents. It’s paramount that the language used in consent forms is clear and comprehensible to foster informed decision-making.
Components of a consent form
Steps to complete a consent to treatment form
Completing a consent to treatment form involves several actionable steps designed to inform and empower patients thoroughly.
Step 1: Preparing the patient
Prior to presenting the consent form, healthcare providers should prepare the patient for their treatment journey. Educating patients about the nature of their condition and the proposed interventions establishes a trusting relationship and lays the groundwork for informed decision-making.
Step 2: Providing adequate information
Healthcare providers must furnish patients with comprehensive information about their treatment options, including risks and benefits. This approach helps create a well-rounded perspective and facilitates informed choices by equipping patients with all necessary knowledge.
Step 3: Allowing time for questions
An open dialogue is crucial in the consent process. Patients should feel encouraged to ask questions and voice doubts. This interaction not only reassures patients but also enables healthcare providers to clarify any misconceptions, further ensuring patients are truly informed.
Step 4: Completing the form
After the discussions, patients should be guided to complete the consent form accurately. Providers should ensure that they understand each section of the form. When patients refuse to sign a consent form, it’s essential to document this refusal carefully, addressing any concerns they may have in a follow-up discussion.
Step 5: Documenting the process
Keeping detailed records of consent discussions and the signed forms is a best practice. This documentation supports accountability and demonstrates that healthcare providers have complied with legal requirements, safeguarding both parties in the event of any future disputes.
Best practices for using consent forms
To maximize the effectiveness of consent forms, healthcare providers should adopt best practices that ensure compliance and clarity.
Regular updates and reviews
Healthcare regulations continually evolve, and so should consent forms. Regularly reviewing and updating these documents ensures they remain compliant with current laws, protecting providers and enhancing patient understanding.
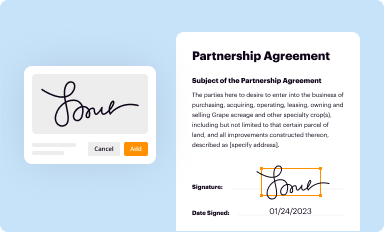
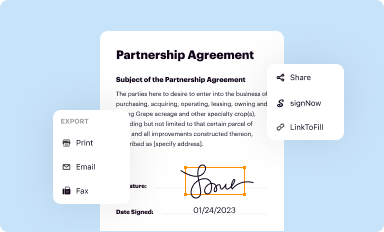
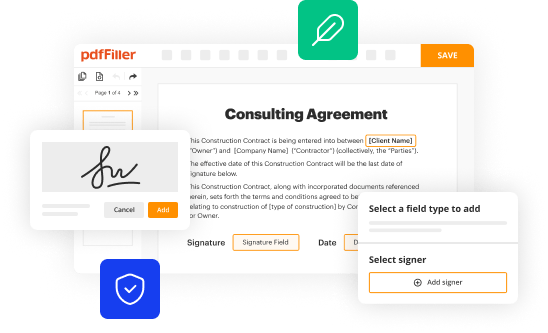
Digital consent solutions: Benefits and features
Using digital solutions like pdfFiller streamlines the consent process significantly. With features such as online editing, e-signatures, and cloud storage, digital consent forms enhance efficiency and provide secure access whenever needed. This approach reduces paperwork and fosters an environmentally friendly practice.
Ensuring accessibility
Consent forms should be easily accessible for both patients and healthcare staff. Placing these forms within a centralized digital system like pdfFiller ensures that everyone involved has quick access to necessary documents, optimizing the consent process and allowing for prompt decision-making when it is most critical.
Interactive tools for managing consent processes
Employing interactive tools can greatly improve how healthcare providers manage consent processes, making them smoother and more effective.
Using pdfFiller for consent forms
pdfFiller offers numerous features that simplify the management of consent forms. Users can easily edit, fill, and sign documents online. This accessibility means that healthcare providers can obtain essential permissions quickly, ensuring a seamless patient experience without the delays associated with paper forms.
Collaborating on forms
Teams can cooperate efficiently on consent documents within the pdfFiller platform. By allowing multiple team members to review and edit forms, healthcare facilities can streamline the approval processes while maintaining compliance with necessary regulations.
Data security and compliance
PDFFiller ensures that all documents managed within the platform are secure and compliant with relevant healthcare data regulations. Encrypting consent forms and safeguarding patient data builds trust and avoids potential legal ramifications, making this approach not only efficient but also safe.
Conclusion
Properly managed consent is vital in healthcare, safeguarding patient rights while empowering informed choices. The process of obtaining consent to treatment should be thorough, transparent, and respectful, ensuring that patients feel valued and understood. As healthcare continues to evolve in the digital age, effective tools like pdfFiller emerge as critical functions in enhancing patient care.
By emphasizing the importance of consent forms and leveraging modern technology solutions, healthcare providers can not only streamline their processes but also enhance patient experiences and outcomes.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete consent to treatment and online?
Can I create an electronic signature for signing my consent to treatment and in Gmail?
How do I edit consent to treatment and on an iOS device?
What is consent to treatment and?
Who is required to file consent to treatment and?
How to fill out consent to treatment and?
What is the purpose of consent to treatment and?
What information must be reported on consent to treatment and?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.