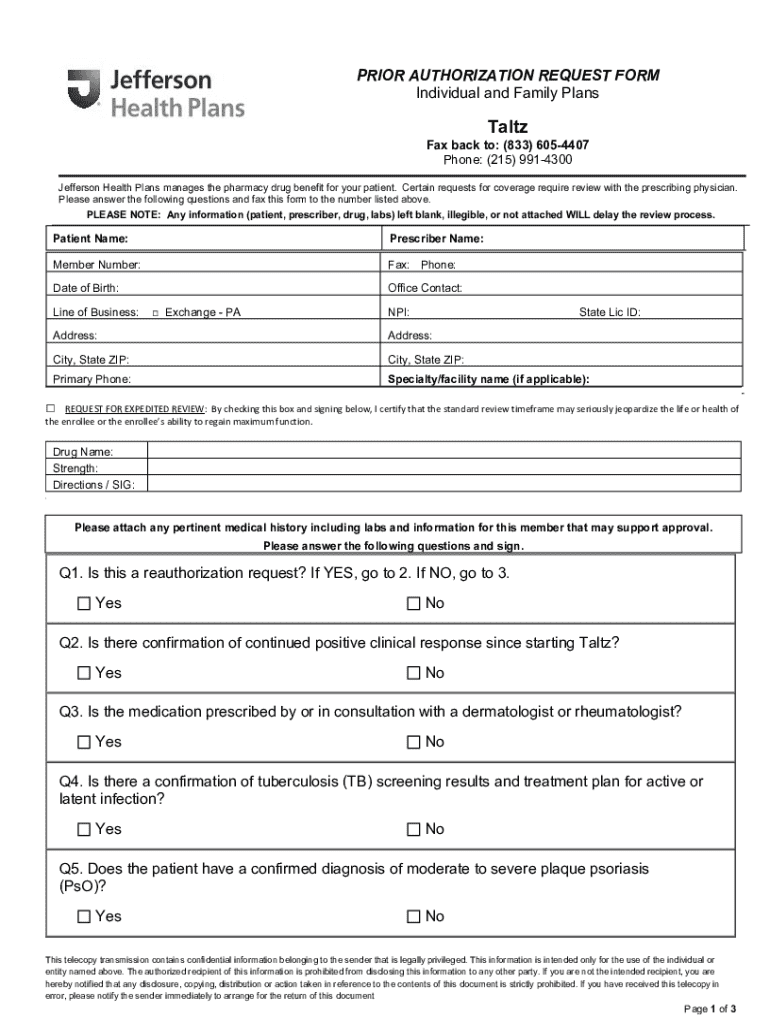
Get the free Prior Authorization Request Form
Get, Create, Make and Sign prior authorization request form
Editing prior authorization request form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization request form
How to fill out prior authorization request form
Who needs prior authorization request form?
Understanding the Prior Authorization Request Form
Understanding the prior authorization process
Prior authorization is a process used by health insurance companies to decide if they will cover a prescribed procedure, service, or medication. This process is essential in controlling health care costs and ensuring that patients receive necessary and appropriate care. Insurance providers require this step to determine the medical necessity of a treatment before it is performed, thus preventing unwarranted expenditures.
In the context of healthcare, prior authorization ensures effective management of resources across insurance plans. It often includes a thorough review by medical professionals who verify that a proposed treatment aligns with clinical guidelines. This step can significantly impact the patient experience, emphasizing the importance of understanding what information is typically needed to streamline the process effectively.
When is prior authorization needed?
Prior authorization is commonly required for certain scenarios, particularly when there is a high cost involved or when the treatment is classified as experimental. For instance, surgeries, advanced imaging studies (like MRIs or CT scans), and specialty medications frequently necessitate prior authorization. Without proper authorization, patients may face substantial out-of-pocket expenses, or worse, denial of coverage entirely.
Failing to obtain the necessary prior authorization can lead to significant delays in treatment. A patient might find themselves in a bind, unable to commence necessary treatments, causing deterioration in their condition. Understanding specific procedures and medications that require prior authorization can empower patients and healthcare providers to navigate these requirements more effectively.
Navigating the prior authorization request form
The prior authorization request form often varies by insurance provider but typically includes several key sections. This section aims to simplify the complex terminology that may be intimidating to patients and healthcare providers. Writing a complete and accurate prior authorization request is critical for swift approval and to ensure that the patient receives the necessary treatment.
Common sections of the form include patient information, provider details, a list of diagnosis codes (ICD codes), and procedure codes (CPT codes). Ensure you have these codes ready, as they are integral to demonstrating the necessity of the proposed treatment.
Step-by-step instructions for completing the form
To complete the prior authorization request form accurately, start by gathering all necessary documentation. Having patient medical records, previous treatment details, and insurance information readily available will make the process smoother. Each section of the form must be filled out thoughtfully. Begin with patient information, which includes contact details and insurance specifics.
Next, you’ll need to document the medical necessity of the treatment thoroughly. This justification is often critical for approval. Include relevant ICD and CPT codes accurately to minimize the chances of rejection. After you’ve completed the form, double-check to ensure all information is consistent and complete before submission to avoid unnecessary delays.
Submission and follow-up process
Submitting the prior authorization request can vary based on the insurance provider. Options typically include mail, fax, and online submissions. It’s essential to be aware of the required method as it can affect the speed of processing your request. Once submitted, you can expect review timelines to vary, commonly ranging from a few days to a couple of weeks, depending on the insurance company's policies.
After submission, be prepared for potential outcomes. Approval will lead to the next steps for treatment, while denials will require further action. Following up on your request is crucial; you should have specific contact points for inquiries. Keeping records of all communications can also significantly streamline the follow-up process.
Common challenges and solutions
Navigating the prior authorization process can be fraught with challenges, particularly when it comes to denials. Understanding the common reasons for denials, such as incomplete information or insufficient justification, can aid in preventing setbacks. If your request is denied, there are methods to appeal the decision; often, this requires additional documentation or a more detailed explanation of medical necessity.
Being proactive in gathering comprehensive documentation from the outset can minimize issues later. Keeping in communication with the insurance provider can also be beneficial, as you can often resolve doubts before they result in a formal denial. Understanding the ins-and-outs of the appeal process can lead to quicker resolutions for denied requests.
Using pdfFiller for your prior authorization needs
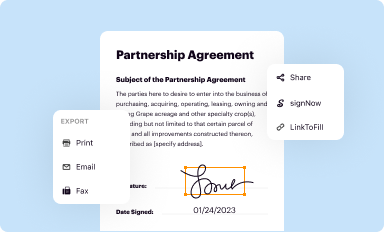
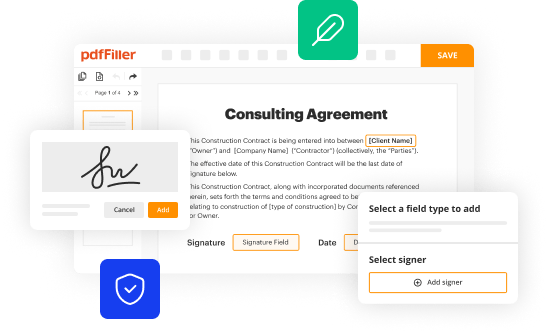
pdfFiller simplifies the prior authorization process with easy access to the necessary forms. Users can access the prior authorization request form via pdfFiller by following straightforward steps. Simply log into your account, navigate to the 'Templates' section, and search for the prior authorization request form you need. The ability to edit and customize the forms directly in your browser removes the hassle of printing and mailing hard copies.
Additionally, pdfFiller’s cloud-based platform allows for seamless collaboration between healthcare providers and patients, ensuring all parties have access to the most current documents. By utilizing tools such as e-signing and various sharing options, managing critical authorization requests becomes a streamlined process.
Additional tools and tips for success
Utilizing interactive templates found within pdfFiller can significantly enhance your document management process. These templates often come pre-populated with useful information and can help in reducing errors when filling out forms. Moreover, implementing best practices by organizing documents efficiently and maintaining good record-keeping habits will boost your productivity and effectiveness in handling prior authorization requests.
Regular reviews of your documentation process can reveal areas for improvement. It's beneficial to create a checklist for required information and documentation to ensure that you are prepared for future prior authorization requests. Moreover, consistent follow-up practices can enhance communication and facilitate a smoother authorization experience.
FAQs about prior authorization requests
In navigating prior authorization requests, many questions arise concerning the process. Common queries often involve timelines for approval, the impact of missing information, and making changes post-submission. Understanding these aspects will empower you to manage expectations and reduce anxiety surrounding prior authorization requests.
Expert guidance clarifies these concerns, providing insight into common misconceptions regarding the prior authorization process. For instance, some believe that all treatments should automatically be covered if requested, but insurance companies typically review claims based on medical necessity and policy coverage, which is why prior authorization is crucial.
Real-life testimonials and case studies
Real-life experiences shed light on the importance of managing prior authorization requests effectively. Users who leverage pdfFiller have reported smoother interactions and faster approvals, highlighting cases where timely submissions have led to improved patient outcomes. Exploring testimonials from individuals who have used pdfFiller can provide a wealth of knowledge and encouragement for those currently navigating the process.
By presenting case studies that emphasize the impact of streamlined authorization processes on patient care, it becomes evident that utilizing effective tools for managing these requests is critical. Patients who face fewer delays in receiving necessary treatments often report better health outcomes, showcasing the integral role of efficient documentation management.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my prior authorization request form in Gmail?
How can I get prior authorization request form?
How do I fill out prior authorization request form using my mobile device?
What is prior authorization request form?
Who is required to file prior authorization request form?
How to fill out prior authorization request form?
What is the purpose of prior authorization request form?
What information must be reported on prior authorization request form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.