Get the free Catamaran rx prior authorization forms
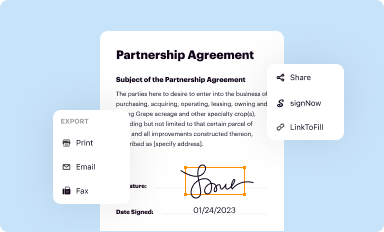
Get, Create, Make and Sign catamaran rx prior authorization
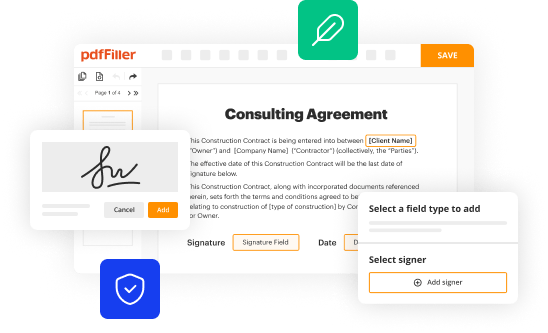
How to edit catamaran rx prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out catamaran rx prior authorization
How to fill out catamaran rx prior authorization
Who needs catamaran rx prior authorization?
Comprehensive Guide to the Catamaran Rx Prior Authorization Form
Overview of the Catamaran Rx Prior Authorization Form
The Catamaran Rx Prior Authorization Form is a critical document used in the healthcare sector to facilitate the prescribing process for certain medications. Its primary purpose is to ensure that healthcare providers obtain necessary approvals from health insurance companies before patients can access specific treatments or drugs. This process is essential to confirm that the prescribed healthcare services or medications are covered and medically appropriate for individual beneficiaries.
Prior authorization serves to manage healthcare costs and maintain optimal patient care. Insurance companies utilize this process to assess whether a requested treatment aligns with established clinical guidelines and whether it is a necessary step within the patient's overall treatment plan. The Catamaran Rx form itself includes key elements such as patient identification details, the specific medication or treatment needing approval, and required clinical information to support the request.
Eligibility criteria for using the Catamaran Rx form
Understanding who needs to submit the Catamaran Rx Prior Authorization Form is crucial for both patients and healthcare providers. Typically, any individual whose health insurance plan requires prior authorization for specific medications must submit this form. Medications that commonly necessitate prior authorization include those on drug formularies marked as non-preferred or those used for certain conditions that are deemed high-cost or specialty drugs. Examples include treatments for chronic conditions such as cancer, rheumatoid arthritis, or multiple sclerosis.
To check eligibility for insurance coverage on particular medications, healthcare providers can take a few essential steps. First, they should review the patient's health plan to identify any medications requiring prior authorization. Second, it’s advisable to consult the insurer's drug formulary, which provides detailed information about covered drugs and those needing authorization. This ensures that both healthcare providers and patients can smoothly navigate the authorization process and avoid unexpected delays.
Applying for prior authorization: Step-by-step guide
Applying for prior authorization using the Catamaran Rx form involves several critical steps. The first step is to gather all necessary patient information. This includes collecting patient identification details such as name, date of birth, and insurance information, including policy number and group ID. Having accurate patient information at hand is vital to avoid errors and expedite the authorization process.
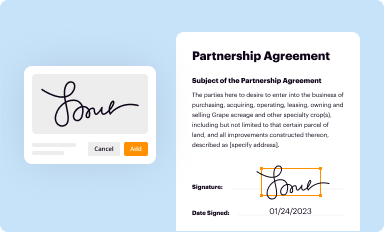
Next, you’ll want to download the Catamaran Rx Form. The form is readily accessible online, particularly on platforms like pdfFiller. Users can easily navigate to the website, search for the Catamaran Rx Prior Authorization Form, and download it in a PDF format. Once you have the form, you’ll need to complete it, paying careful attention to specific sections like the patient's medical history, current medications, and the requested treatment.
The submission process comes next, requiring you to decide where to send the completed form. Submissions can typically be made via fax or electronic transmission, each having its pros and cons. Fax submissions are straightforward and may provide immediate confirmation of receipt, whereas electronic submissions often integrate better into the healthcare provider's office workflow.
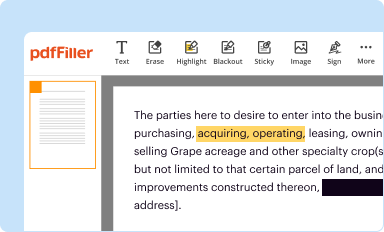
Tools and features for seamless form filling on pdfFiller
Utilizing pdfFiller for completing the Catamaran Rx Prior Authorization Form offers users significant advantages. One prominent advantage is the interactive form fields that allow for seamless data entry without the hassle of manually filling out a paper form. This feature reduces the likelihood of errors and significantly speeds up the completion process.
Additionally, pdfFiller offers options for editing and saving the form, allowing users to revisit it as needed before final submission. The platform also supports collaboration among team members, enhancing communication and allowing different stakeholders, such as prescribers and healthcare professionals, to contribute essential information to the form.
Understanding the review process
After submission, healthcare providers may wonder what happens next in the review process. Typically, health insurance companies have a specific timeline for reviewing prior authorization requests, which can range from as little as 24 hours to several days, depending on the complexity of the authorization. During this time, insurance representatives will review the submitted documentation and assess whether the requested treatment aligns with their coverage guidelines.
To check the status of a submission, many insurers provide online portals where providers can log in to see real-time updates on the authorization request. This transparency can greatly reduce stress for both patients and healthcare providers and allows for timely adjustments to treatment plans based on the insurer's response.
Handling denials and appeals
Denials for prior authorization requests can be frustrating, but understanding common reasons can help in preparing a stronger application. Typical reasons for denial include incomplete submissions, lack of medical necessity, or the treatment being outside the prescribed formulary. When faced with a denial, it’s critical to understand how to navigate the appeals process.
To initiate an appeal, healthcare providers should first review the denial letter for specific reasons and gather necessary documentation that supports the medical necessity of the requested treatment. This often involves updating the original authorization form and including relevant clinical notes or additional tests that justify the treatment. Providers should then follow the insurer's specified appeal process, which may include submitting additional paperwork or scheduling a review meeting.
Additional related forms
In addition to the Catamaran Rx Prior Authorization Form, healthcare providers may encounter other authorization forms necessary for various treatments or medications. For instance, Optum Rx offers its authorization forms, and healthcare professionals should familiarize themselves with these as these may have differing requirements.
Another form to consider is the Step Therapy Exemption Form, which may be necessary for patients who have previously tried and failed other treatment options. By understanding the range of available authorization forms and their specific requirements, both healthcare providers and patients can better navigate the reimbursement landscape. Accessing these related documents can often be facilitated through platforms like pdfFiller, providing a centralized solution for all form needs.
Frequently asked questions (FAQs)
Frequently asked questions surrounding the Catamaran Rx Prior Authorization Form contribute to a better understanding of its use. For instance, many individuals wonder what to do if they need assistance filling out the form. In such cases, healthcare providers or support staff can guide patients through the process, ensuring that all necessary fields are filled accurately. Additionally, users often ask if they can make changes to the form after submission; in general, while alterations are possible, contacting the insurer directly is advisable for optimal procedure adherence.
For those seeking further assistance, contacting the customer support team of the insurance provider is crucial. They can provide additional insights and clarification regarding the authorization process, along with updates on the current status of submitted forms.
User experiences and testimonials
Real-world experiences with the Catamaran Rx Prior Authorization Form reveal how important it is to have a well-organized process. Many healthcare professionals have shared success stories about how timely submission of this form led to swift approvals for critical medications. These testimonials highlight the benefits of being proactive and thorough in the preparatory steps before submission.
Beyond individual experiences, feedback regarding the use of pdfFiller for completing administrative tasks reveals a trend toward enhanced efficiency and teamwork. Users praise the platform for its intuitive layout, which simplifies the process of filling out, eSigning, and managing documents, allowing healthcare teams to focus more on patient care and less on administrative hurdles.
Further learning and resources
For those looking to deepen their understanding of the Catamaran Rx Prior Authorization Form, video tutorials are an invaluable resource. These short, instructional videos guide users through the process of filling out the form, identifying common pitfalls, and presenting effective strategies for successful submission.
Moreover, various articles and guides are available that provide additional insights into navigating the authorization landscape. Engaging with these resources can empower healthcare providers and patients to make more informed decisions. Reaching out to provider resources that specialize in authentication and support further enhances the ability to manage paperwork efficiently, ensuring every patient receives the necessary care seamlessly.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make edits in catamaran rx prior authorization without leaving Chrome?
Can I create an eSignature for the catamaran rx prior authorization in Gmail?
How do I edit catamaran rx prior authorization on an Android device?
What is catamaran rx prior authorization?
Who is required to file catamaran rx prior authorization?
How to fill out catamaran rx prior authorization?
What is the purpose of catamaran rx prior authorization?
What information must be reported on catamaran rx prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.