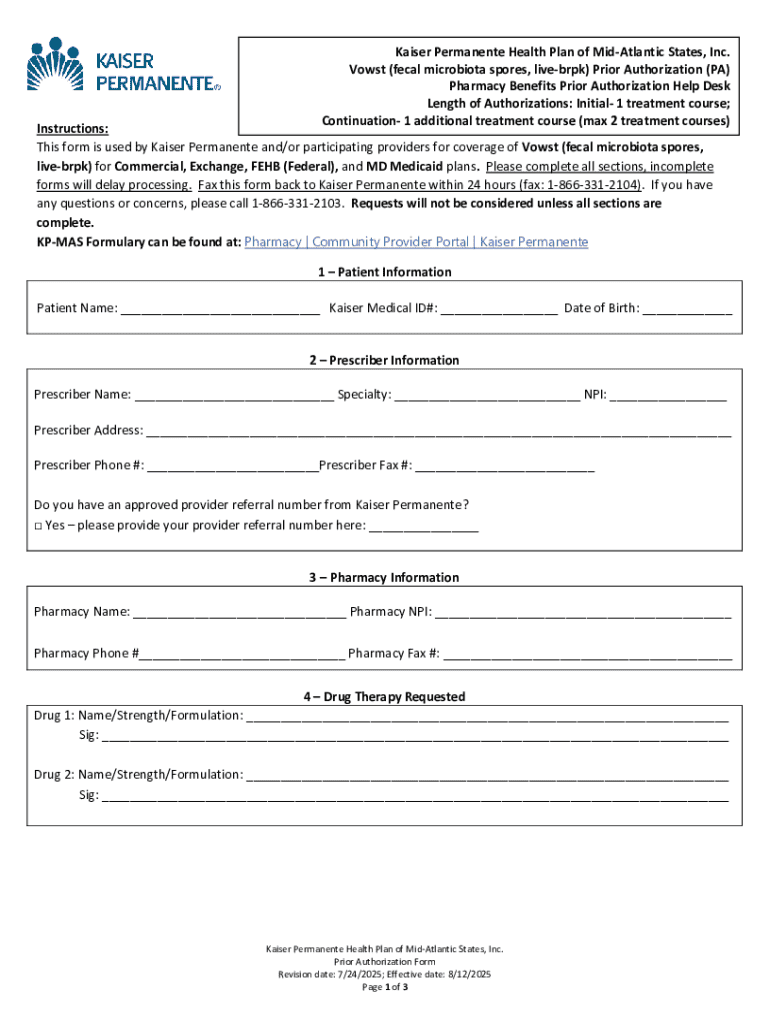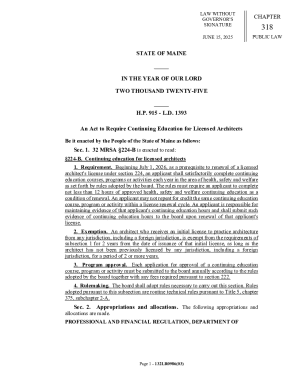
Get the free Prior Authorization (PA) Form for Vowst (fecal microbiota spores, live ...
Get, Create, Make and Sign prior authorization pa form
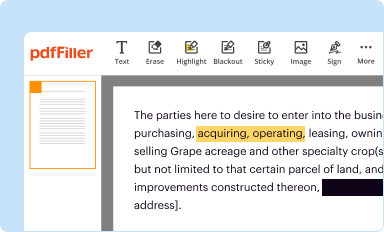
How to edit prior authorization pa form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization pa form
How to fill out prior authorization pa form
Who needs prior authorization pa form?
Understanding the Prior Authorization PA Form: A Comprehensive Guide
Understanding prior authorization
Prior authorization (PA) serves as a critical step in determining the medical necessity and appropriateness of certain healthcare services or medications before they are delivered to patients. The process helps insurance companies assess whether the proposed treatment aligns with their coverage policies, with the primary goal of controlling costs and ensuring quality care.
In the U.S. healthcare system, prior authorization plays a significant role in maintaining a balance between patient care and cost management. This mechanism helps prevent unnecessary procedures and preserves healthcare resources. Medical procedures, high-cost medications, and certain specialized treatments often require prior authorization to be eligible for payment.
The behavior of insurance companies towards prior authorization varies widely. Some insurers have streamlined processes that facilitate quicker approvals, while others may take longer and complicate the process with additional documentation requirements. Understanding the policies and procedures of your specific insurer is crucial for smooth navigation through the prior authorization landscape.
Before filling out the prior authorization PA form
Before diving into the specifics of the prior authorization PA form, there are critical preparatory steps to ensure that the process goes as smoothly as possible. Start by gathering essential details about the patient, the provider, and the requested treatment.
Moreover, it’s critical to review your insurance requirements before completing the form. Each insurance plan has different criteria for coverage; thus, understanding what is encompassed within your policy is essential to avoid unnecessary denials. Common reasons for denial may include failure to establish medical necessity or not adhering to facility-specific protocols.
Detailed guide to completing the PA form
Completing the prior authorization PA form involves several key steps. Accuracy and thoroughness are vital to increasing the likelihood of approval. Follow this step-by-step guide to ensure you cover all necessary elements.
Pay attention to ensure the accuracy of your entries. Common mistakes include typographical errors, incomplete information, and missing documentation. Double-check everything before submission to reduce the chances of setbacks. Mistakes could cost valuable time in the approval process or even lead to outright denial.
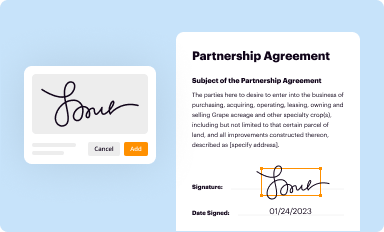
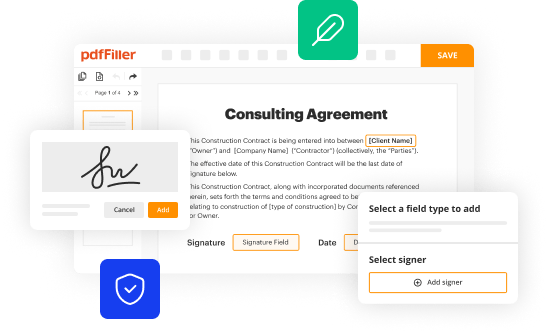
Using pdfFiller's tools for your PA form
pdfFiller offers a suite of interactive tools designed to enhance your experience while filling out the prior authorization PA form. These capabilities make the process not only simpler but also more efficient.
Utilizing pdfFiller, you can seamlessly complete the entire PA form and manage your documents effectively. This ensures an organized workflow and a much simpler experience when navigating complex forms.
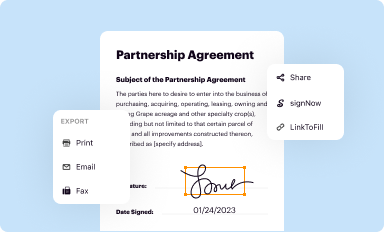
Submitting your prior authorization PA form
Once your prior authorization PA form is complete, it’s time for submission. Knowing where and how to submit your form is instrumental in facilitating timely reviews. Many insurance companies now offer online submission options, making the process more efficient.
After submitting your PA form, tracking the submission is essential. Many providers offer tracking options, so be proactive in checking the status of your request. Typical response times may vary depending on the insurer, so be prepared for varying timelines.
Frequently faced challenges and solutions
Navigating prior authorization can pose several challenges, and being prepared can help mitigate these obstacles. Among the most common issues are delayed responses from insurers and repeated denials of requests.
Best practices for overcoming these challenges include establishing efficient communication channels with your insurer and knowing when to appeal a denial after thoroughly understanding the reasons and clarifying them with all necessary documentation.
Understanding outcomes and next steps
After submitting your prior authorization PA form, the request undergoes a review process within the insurance company. They will typically notify you or your provider if the request has been approved or denied. It's crucial to understand the potential outcomes and next steps that follow.
This proactive approach allows patients and providers to navigate the healthcare system efficiently, ensuring continuity of care.
Leveraging pdfFiller for document management
Employing a cloud-based solution like pdfFiller offers significant benefits in managing your prior authorization PA form and other necessary documents. Cloud storage simplifies access and enhances the security of sensitive documents.
Moreover, version control features help maintain the integrity of documents, allowing users to revert to previous iterations if needed.
Enhancing collaboration with your healthcare team
Collaboration between healthcare providers can significantly improve patient outcomes. Sharing the prior authorization PA form with team members increases visibility and enables better coordination of patient care.
Coordinating with different healthcare providers allows for a streamlined approach that minimizes the risk of miscommunication, ensuring patients receive the comprehensive care they need.
FAQs about prior authorization
Navigating the world of prior authorization begs several common questions. Below are clarifications for frequently asked inquiries.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send prior authorization pa form to be eSigned by others?
Can I create an electronic signature for the prior authorization pa form in Chrome?
Can I edit prior authorization pa form on an iOS device?
What is prior authorization pa form?
Who is required to file prior authorization pa form?
How to fill out prior authorization pa form?
What is the purpose of prior authorization pa form?
What information must be reported on prior authorization pa form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.