Get the free does tricare cover vyvanse form
Show details
Share. NOTE: This form applies to. A separate form applies to, and XR. ? You do NOT need to complete this form in order for ...
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign
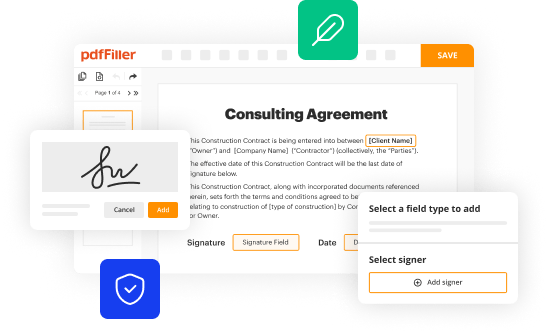
Edit your does tricare cover vyvanse form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your does tricare cover vyvanse form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit does tricare cover vyvanse online
Follow the guidelines below to use a professional PDF editor:
1
Create an account. Begin by choosing Start Free Trial and, if you are a new user, establish a profile.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit tricare vyvanse form. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Get your file. Select your file from the documents list and pick your export method. You may save it as a PDF, email it, or upload it to the cloud.
pdfFiller makes dealing with documents a breeze. Create an account to find out!
How to fill out does tricare cover vyvanse
How to fill out tricare vyvanse prior authorization?
01
Contact your healthcare provider: Reach out to your healthcare provider and discuss your need for Vyvanse medication. They will evaluate your condition and determine if Vyvanse is the appropriate treatment option for you.
02
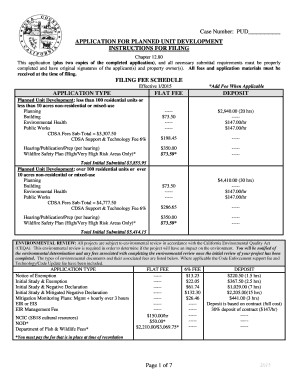
Obtain the necessary forms: Ask your healthcare provider for the tricare vyvanse prior authorization form. They will provide you with the required paperwork to initiate the authorization process.
03
Fill out the form accurately: Take your time to complete the tricare vyvanse prior authorization form diligently. Provide all the necessary information such as your personal details, medical history, and diagnosis supporting the need for Vyvanse treatment. Be sure to include any relevant documentation or test results, if required.
04
Include supporting documents: Attach any supporting documents that may help in justifying the need for Vyvanse treatment. This may include medical records, test results, or letters from healthcare professionals. Ensure that these documents are legible and organized.
05
Submit the form: Once you have completed the form and gathered all necessary attachments, submit the tricare vyvanse prior authorization form to the appropriate authority. This may be your insurance company or a designated review board. Follow the submission instructions provided by your healthcare provider or the authorization body.
06
Follow up: Track the progress of your prior authorization request. Contact your insurance company or the designated reviewing authority to inquire about the status of your application. They will provide you with updates regarding the approval or denial of your vyvanse prior authorization request.
Who needs tricare vyvanse prior authorization?
01
Patients seeking Vyvanse treatment: Individuals who are considering Vyvanse as a treatment option for their medical condition may need to undergo the tricare vyvanse prior authorization process to ensure coverage and reimbursement.
02
Healthcare providers: Physicians, psychiatrists, or other healthcare professionals prescribing Vyvanse may need to initiate the tricare vyvanse prior authorization process on behalf of their patients. This authorization ensures that the treatment is deemed appropriate and necessary before being covered by insurance.
03
Insurance companies or designated reviewing authorities: Insurance companies or designated review boards are responsible for evaluating the tricare vyvanse prior authorization requests. They review the submitted forms, assess the supporting documentation, and determine whether or not to approve the request based on their coverage criteria and guidelines.
Fill tricare medical necessity form pdf : Try Risk Free
People Also Ask about does tricare cover vyvanse
Does TRICARE pay for Vyvanse?
How do I check my TRICARE authorization status?
How long does it take for TRICARE to approve prior authorization?
How do I submit a prior authorization to TRICARE?
How do I get a prior authorization from TRICARE?
How long does it take to get a pre authorization from TRICARE?
What ADHD medication does TRICARE cover?
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is tricare vyvanse prior authorization?
Tricare Vyvanse prior authorization refers to the process that members of the Tricare health insurance program must undergo in order to receive coverage for the prescription medication Vyvanse. Vyvanse is a medication used to treat attention deficit hyperactivity disorder (ADHD) in both children and adults.
Tricare is a health insurance program for uniformed service members, retirees, and their families. Prior authorization is a requirement by insurance providers that ensures a medication's necessity and appropriateness before it will be covered. It is a way for insurance companies to control costs and ensure that medications are being used for their intended purpose.
To obtain coverage for Vyvanse, a Tricare member must have their healthcare provider submit a request for prior authorization. This process may involve submitting supporting documentation, such as medical records, to demonstrate the medical necessity of the medication.
Once the prior authorization request is reviewed and approved by Tricare, the member can then receive coverage for Vyvanse, allowing them to obtain the medication at a lower cost or no cost at all, depending on their specific Tricare plan.
Who is required to file tricare vyvanse prior authorization?
The healthcare provider is typically responsible for filing the Tricare Vyvanse prior authorization. This involves submitting the necessary documentation and information to support the medical necessity of prescribing Vyvanse for the patient. The patient may also need to provide certain information, such as medical history or documentation from previous treatments, to assist with the prior authorization process.
How to fill out tricare vyvanse prior authorization?
To fill out a TRICARE Vyvanse prior authorization, follow these steps:
1. Obtain the prior authorization form: Visit the TRICARE website or contact your TRICARE provider to obtain the necessary prior authorization form. Ensure that you have the latest version of the form.
2. Review the form: Carefully read through the prior authorization form to understand the information required and the supporting documentation that needs to be submitted. Make sure you have all the necessary documents before starting the application.
3. Gather required information: Collect the required information to complete the form. This may include the beneficiary's name, TRICARE ID number, prescribing doctor's information, medication details (such as dosage and frequency), and medical history.
4. Complete the form: Fill in all the necessary fields on the prior authorization form. Be sure to provide accurate details and double-check for any errors or missing information. Some sections may require a signature, so ensure you and your healthcare provider sign where necessary.
5. Attach supporting documents: Gather any supporting documents required for the prior authorization. This may include medical records, test results, or a letter of medical necessity from your healthcare provider. Review the form instructions to ensure you include all the necessary documentation.
6. Submit the prior authorization: Once the form is complete and you have attached all the required documents, submit the prior authorization to the appropriate TRICARE office or the designated address mentioned in the instructions. Some forms may also allow for online submission, so check for any available electronic submission options.
7. Follow up: After submitting the prior authorization, follow up with TRICARE to ensure it has been received and is being processed. Note any reference number or confirmation details provided during submission, as these may be useful for tracking the progress of your request.
Remember to keep copies of all documents submitted and take note of any relevant dates or deadlines throughout the process.
What is the purpose of tricare vyvanse prior authorization?
The purpose of Tricare Vyvanse prior authorization is to ensure that the use of the medication Vyvanse is appropriate and medically necessary for the individual seeking coverage under the Tricare health insurance program. Prior authorization is a process where the prescribing healthcare provider must demonstrate that the patient meets certain criteria and justifies the need for Vyvanse before Tricare will cover the medication. This helps control costs, prevent unnecessary or inappropriate use of the medication, and ensures that the medication is being prescribed in accordance with Tricare's guidelines and policies.
What information must be reported on tricare vyvanse prior authorization?
To obtain prior authorization for Vyvanse through Tricare, the following information may need to be reported:
1. Patient Information: Full name, date of birth, Tricare beneficiary number, contact information.
2. Prescriber Information: Name, contact information, specialty, National Provider Identifier (NPI).
3. Diagnosis: The specific diagnosis for which Vyvanse is being prescribed.
4. Medication Information: Name of the medication (Vyvanse), dosage, strength, quantity, directions for use.
5. Medical Necessity: A detailed explanation of why Vyvanse is necessary for the patient's medical condition and how it will improve their health outcome.
6. Treatment Plan: An overview of the treatment plan, including any other medications or interventions that have been tried or considered.
7. Relevant Clinical Documentation: Any supporting documentation, such as medical records, test results, or progress notes, that demonstrate the need for Vyvanse.
8. Duration of Treatment: The requested duration of treatment with Vyvanse.
9. Prior Medication History: A record of any previous medications tried for the condition and their effectiveness, including any adverse reactions.
Please note that specific documentation requirements may vary depending on the Tricare program and the individual patient's circumstances. It is always recommended to consult the Tricare provider manual or contact the Tricare customer service for the most accurate and up-to-date information regarding prior authorization requirements.
Can I create an electronic signature for the does tricare cover vyvanse in Chrome?
As a PDF editor and form builder, pdfFiller has a lot of features. It also has a powerful e-signature tool that you can add to your Chrome browser. With our extension, you can type, draw, or take a picture of your signature with your webcam to make your legally-binding eSignature. Choose how you want to sign your tricare vyvanse form and you'll be done in minutes.
Can I create an electronic signature for signing my tricare vyvanse prior authorization form in Gmail?
It's easy to make your eSignature with pdfFiller, and then you can sign your vyvanse coupon tricare right from your Gmail inbox with the help of pdfFiller's add-on for Gmail. This is a very important point: You must sign up for an account so that you can save your signatures and signed documents.
How do I complete vyvanse tricare on an iOS device?
Get and install the pdfFiller application for iOS. Next, open the app and log in or create an account to get access to all of the solution’s editing features. To open your fill vyvanse at my mtf form, upload it from your device or cloud storage, or enter the document URL. After you complete all of the required fields within the document and eSign it (if that is needed), you can save it or share it with others.
Fill out your does tricare cover vyvanse online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Tricare Vyvanse Prior Authorization Form is not the form you're looking for?Search for another form here.
Keywords relevant to tricare and vyvance form
Related to tricare medical necessity form
If you believe that this page should be taken down, please follow our DMCA take down process
here
.