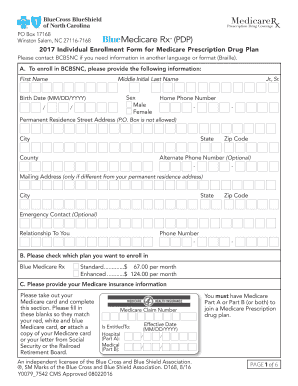
Bcbsnc Prescription Claim Form
What is bcbsnc prescription claim form?
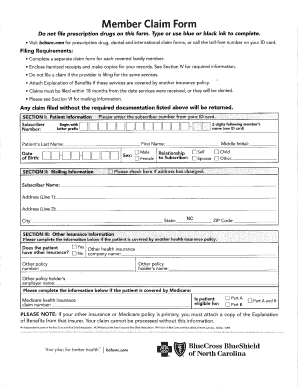
The bcbsnc prescription claim form is a document used by Blue Cross Blue Shield of North Carolina (BCBSNC) members to request reimbursement for prescription medications. This form allows members to provide the necessary information for BCBSNC to process their claim and issue reimbursement.
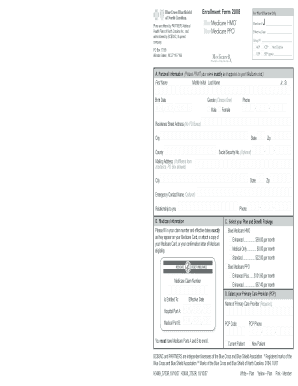
What are the types of bcbsnc prescription claim form?
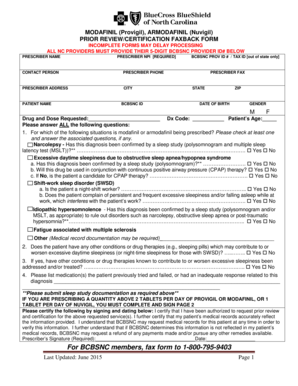
There are different types of bcbsnc prescription claim forms available based on the specific needs of the member. The most commonly used types include: 1. Standard Prescription Claim Form: This form is used for general reimbursement requests. 2. Specialty Medication Claim Form: This form is used for specialty medications that require additional information. 3. Mail Order Pharmacy Claim Form: This form is used for reimbursement requests related to mail-order pharmacy services. 4. Prior Authorization Exception Request Form: This form is used to request authorization for medications that require prior approval. 5. Coordination of Benefits (COB) Prescription Claim Form: This form is used when a member has primary coverage with another insurance provider.
How to complete bcbsnc prescription claim form
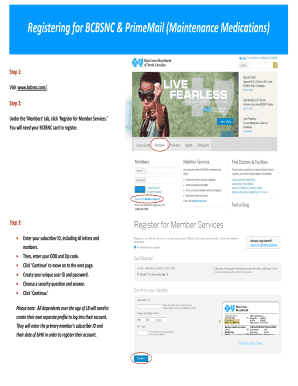
Completing the bcbsnc prescription claim form is a straightforward process. Here are the steps involved: 1. Download the appropriate claim form from the BCBSNC website or obtain a physical copy from your healthcare provider. 2. Fill in your personal information, including your name, address, and BCBSNC member ID. 3. Provide details about the prescription medication, including the name, dosage, and quantity. 4. Attach the original pharmacy receipt and a copy of the prescription. 5. Sign and date the form. 6. Submit the completed form along with supporting documents to BCBSNC for review and processing.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.