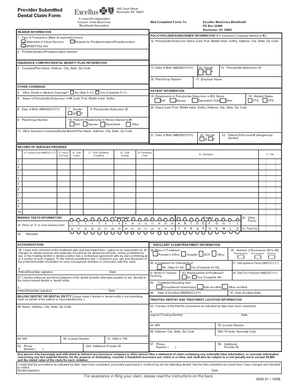
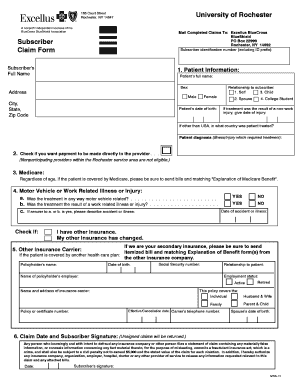
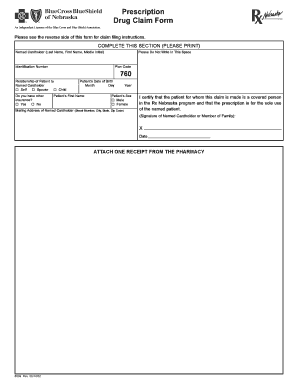
Blue Cross Blue Shield Association Member Claim Form
What is Blue Cross Blue Shield Association Member Claim Form?
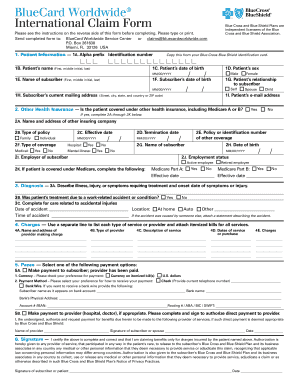
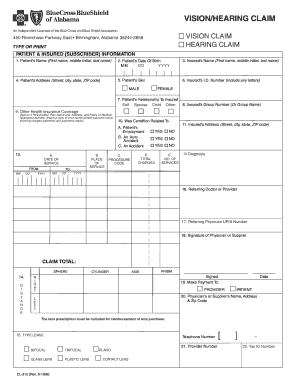
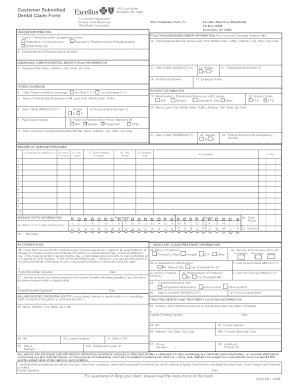
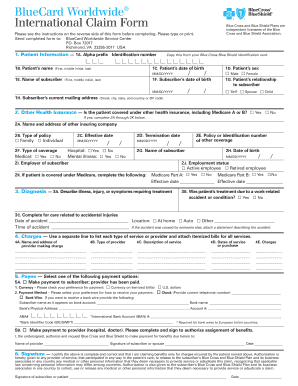
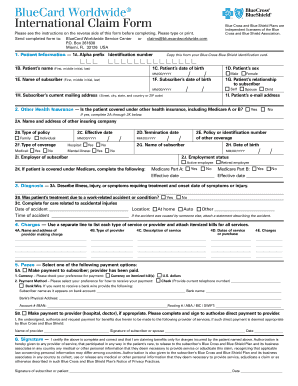
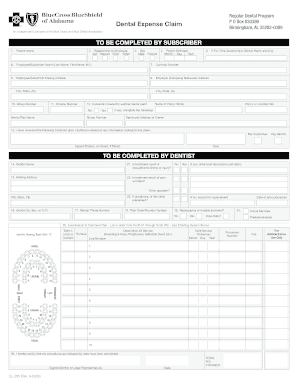
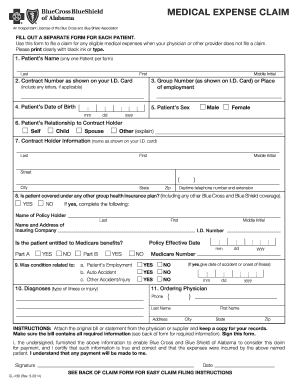
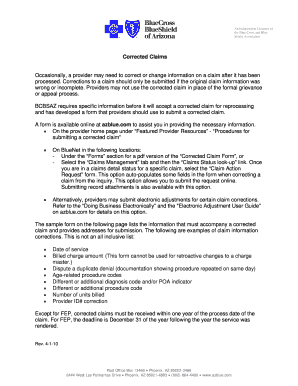
The Blue Cross Blue Shield Association Member Claim Form is a document used by Blue Cross Blue Shield Association members to request reimbursement for medical services. It allows members to submit claims for healthcare expenses incurred outside of their network or for services that are not covered by their insurance policy.
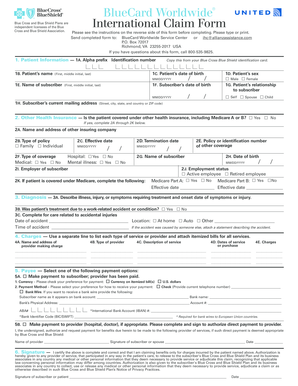
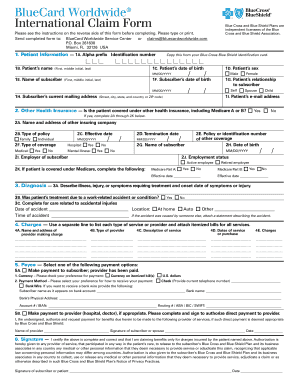
What are the types of Blue Cross Blue Shield Association Member Claim Form?
There are two main types of Blue Cross Blue Shield Association Member Claim Forms:
How to complete Blue Cross Blue Shield Association Member Claim Form
Follow these steps to complete the Blue Cross Blue Shield Association Member Claim Form:
By using pdfFiller, members can easily create, edit, and share their Blue Cross Blue Shield Association Member Claim Forms online. With unlimited fillable templates and powerful editing tools, pdfFiller is the ultimate PDF editor for getting documents done efficiently.