Hospital Discharge Summary Requirements
What is hospital discharge summary requirements?
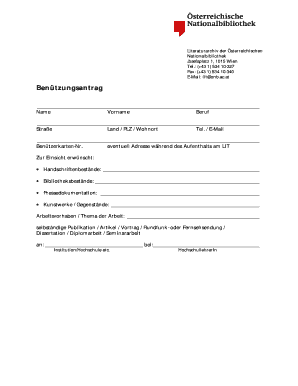
A hospital discharge summary is a document that outlines the medical information and instructions provided to a patient upon their release from the hospital. It serves as a comprehensive record of the patient's hospital stay, including their diagnosis, treatment, and follow-up care. The discharge summary is an essential part of the healthcare process, as it ensures continuity of care and provides important information for both the patient and their healthcare providers.
What are the types of hospital discharge summary requirements?
There are several types of hospital discharge summary requirements that may vary depending on the healthcare facility and the specific needs of the patient. Some common types include:
How to complete hospital discharge summary requirements
Completing hospital discharge summary requirements requires careful attention to detail and thorough documentation. Here are the steps to follow:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.