What is sample nurses notes narrative?
Sample nurses notes narrative refers to the written documentation recorded by nurses to document their observations and assessments of a patient's condition, as well as the care provided. It includes details about the patient's vital signs, symptoms, treatment administered, and any changes observed. These notes serve as an essential communication tool among healthcare providers and ensure continuity of care for the patient.
What are the types of sample nurses notes narrative?
There are several types of sample nurses notes narratives, each serving a specific purpose in documenting patient care. Some common types include:
Admission notes: These are written when a patient is admitted to a healthcare facility and provide an overview of the patient's initial condition.
Progress notes: These are documented regularly to capture the ongoing progress or changes in the patient's condition, including responses to treatment.
Shift notes: These are written at the end of each nursing shift to inform the incoming nurses about the patient's condition, events that occurred, and any interventions.
Discharge notes: These are prepared when a patient is discharged and summarize the care provided during the hospital stay, including instructions for further treatment or follow-up.
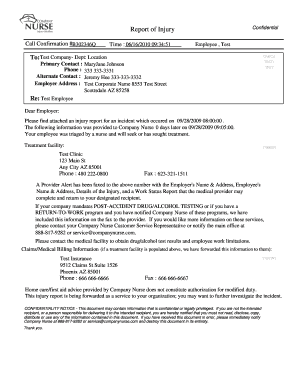
Incident or event notes: These are recorded when unexpected incidents or events occur during patient care, such as falls, medication errors, or adverse reactions.
Nursing care plans: These outline the specific nursing interventions and goals for the patient, providing a framework for the nursing care provided.
How to complete sample nurses notes narrative
Completing a sample nurses notes narrative requires attention to detail and accuracy. Here are some steps to follow:
01
Begin by gathering all relevant information about the patient, including their medical history, current medications, and any recent changes or events.
02
Ensure that the notes are concise, objective, and specific. Use clear language and avoid jargon that may be difficult for others to understand.
03
Include vital signs and assessments, such as heart rate, blood pressure, respiratory rate, and temperature. Document any abnormalities or significant changes.
04
Describe the patient's symptoms or complaints in detail, along with any observed changes or improvements.
05
Document all medications administered, including dosage, route, and time. Note any adverse reactions or side effects.
06
Include any nursing interventions performed, such as wound care, patient education, or assistance with activities of daily living.
07
Sign and date the notes to validate their authenticity and provide a timeline of events.
08
Review the notes for accuracy and completeness before finalizing them.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.