What is a SOAP Note?
The SOAP Note is one of the forms utilized in the healthcare industry when collecting all of the data of an admitted patient and comprises a part of the patient’s records.
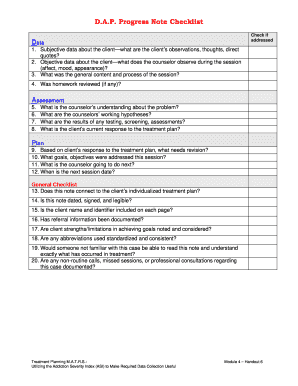
Basically, it’s an acronym where S stands for subjective, O - objective, A - assessment and P - plan. The form can come in different variants and formats depending on the doctor or the patient’s complaints. It can also be used for communication between physicians by adding notes.
For example, if a patient visits another specialist, the documented clinical record gives the specialist an overall idea of the patient’s condition without needing direct contact with the other doctor.
Each point has to be described separately:
Subjective depicts what actually happened, symptoms and history of the disease or injury based on the words of the patient.
The objective is a description from the position of the medical worker who makes a conclusion according to their observation and the results of various medical tests.
Assessment is a probable diagnosis and state of the current problem, for example, whether it's chronic or acute.
The plan is a prescribed treatment. It may be as brief as a receipt or as long as a detailed long-term therapy.
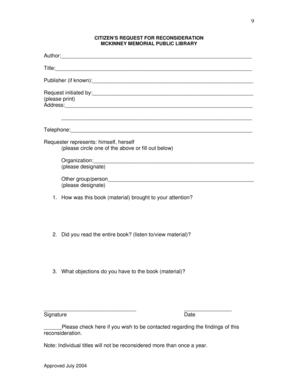
How do I Fill Out a SOAP Notes Form?
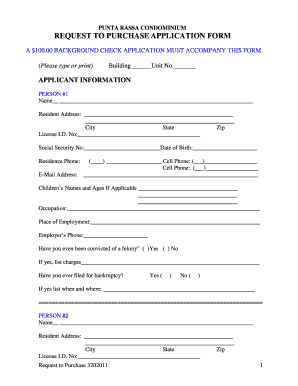
The current s.o.a.p. form is designed for massages in relation to an injury and contains the following parts:
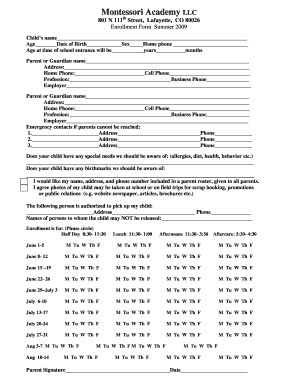
Name of the client, type of massage session, its duration and date.
Insurance ID and information on the treatment: when the injury occurred, type and duration of the treatment and medications applied.
Subjective section - what caused the current condition of the client.
Objective section - what was discovered by the medical worker on the basis of palpation and visual examination.
Assessment - consequences occurred due to the changed condition of the body.
Plan - plan of massage sessions and recommendations for self-care.
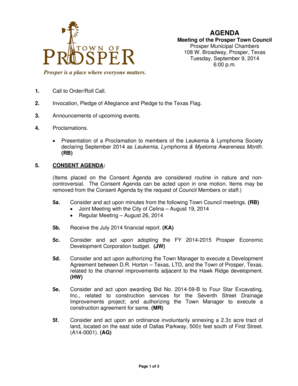
A scheme of a human body and a symbul legend to indicate symptoms such as pain, spasms, inflammation etc.