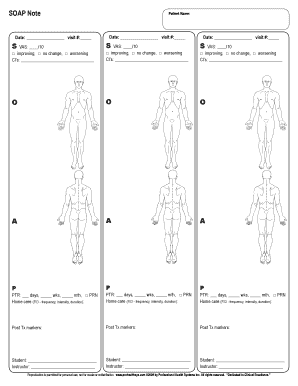
Soap Note Template
What is a SOAP note template?
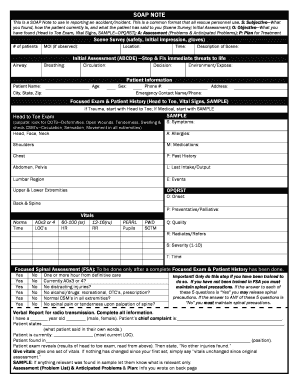
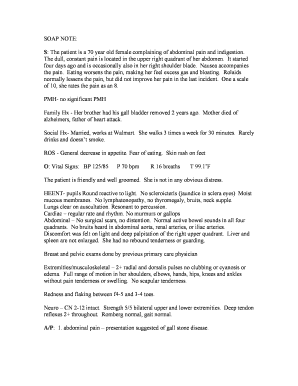
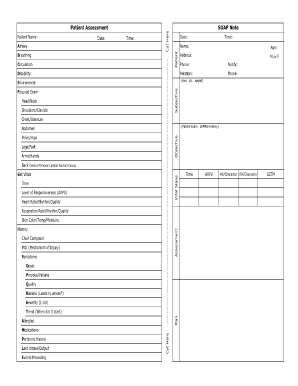
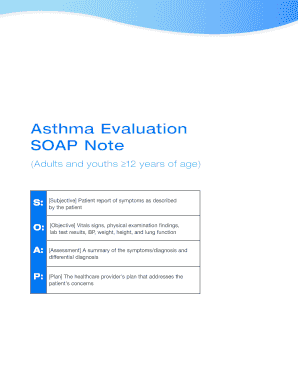
A SOAP note template is a standardized format used by medical professionals to document patient information. SOAP stands for Subjective, Objective, Assessment, and Plan. This template helps healthcare providers organize and communicate patient information effectively to provide comprehensive care.
What are the types of SOAP note templates?
There are several types of SOAP note templates available, each designed for specific medical specialties or purposes. Some common types include:
Medical SOAP note template
Nursing SOAP note template
Physical therapy SOAP note template
Occupational therapy SOAP note template
Mental health SOAP note template
Pediatric SOAP note template
How to complete a SOAP note template
Completing a SOAP note template involves the following steps:
01
Subjective: Document the patient's chief complaint, medical history, and subjective symptoms or concerns.
02
Objective: Record any observable or measurable data such as vital signs, physical examination findings, or laboratory results.
03
Assessment: Provide an assessment or diagnosis based on the collected information and medical knowledge.
04
Plan: Outline the treatment plan, including medications, therapies, follow-ups, and patient education.
05
Document: Ensure the SOAP note is accurate, concise, and in compliance with legal and ethical standards.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.
Video Tutorial How to Fill Out soap note template
Thousands of positive reviews can’t be wrong
Read more or give pdfFiller a try to experience the benefits for yourself
Questions & answers
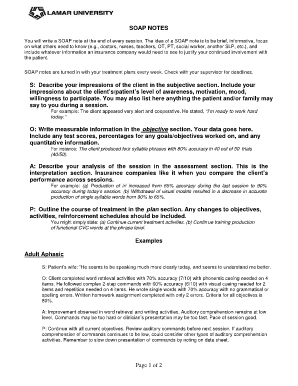
What is soap format of assessment?
The Subjective, Objective, Assessment and Plan (SOAP) is an acronym representing a widely-used method of. documentation in veterinary and human medicine. The SOAP is a way for healthcare workers to document their. thinking in a structured and organized way.[1][2][3]
What are 3 guidelines to follow when writing SOAP notes?
4 tips for writing SOAP notes Don't repeat content from a previous section. Make sure each section has unique content. Don't rewrite your whole treatment plan each time.
What are the 4 parts of soap?
How to Write SOAP Notes. To write a SOAP note, include a section on each of the four elements: Subjective, Objective, Assessment, Plan.
What is soap stand for?
SOAP—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way.
What is the objective part of soap?
The objective section of the SOAP includes information that the healthcare provider observes or measures from the patient's current presentation, such as: Vital signs are often already included in the chart. However, it is an important component of the SOAP note as well. Vital signs and measurements, such as weight.
How do you properly write a SOAP note?
Tips for Effective SOAP Notes Find the appropriate time to write SOAP notes. Maintain a professional voice. Avoid overly wordy phrasing. Avoid biased overly positive or negative phrasing. Be specific and concise. Avoid overly subjective statement without evidence. Avoid pronoun confusion. Be accurate but nonjudgmental.
Related templates