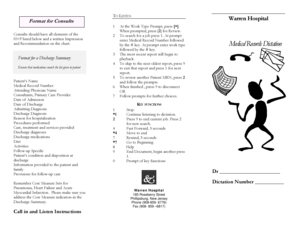
Suggested Discharge Summary Format
What is Suggested Discharge Summary Format?
A Suggested Discharge Summary Format is a standardized template used in healthcare settings to document and communicate a patient's medical history, treatment, and follow-up care after a hospital stay. It serves as a comprehensive summary to ensure continuity of care between healthcare providers.
What are the types of Suggested Discharge Summary Format?
There are various types of Suggested Discharge Summary Formats that healthcare providers may use. Some common types include:
Standard Discharge Summary Format
Customizable Discharge Summary Format
Electronic Discharge Summary Format
Structured Discharge Summary Format
How to complete Suggested Discharge Summary Format
Completing a Suggested Discharge Summary Format involves several key steps:
01
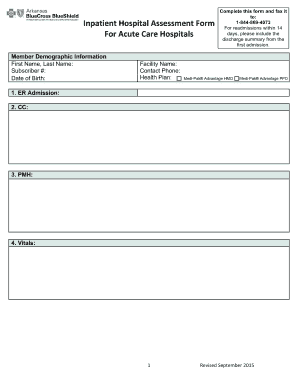
Gather all relevant patient information, including medical history, medications, and procedures performed.
02
Document the reason for admission, diagnosis, treatment provided, and any complications or special considerations.
03
Include a detailed plan for follow-up care, including medication instructions, referrals to specialists, and any necessary post-hospitalization tests or examinations.
04
Ensure accurate and clear documentation of the patient's current condition and any pertinent findings from tests or examinations.
05
Review and verify all information for accuracy and completeness.
06
Share the completed discharge summary with the appropriate healthcare providers and the patient.
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.
Video Tutorial How to Fill Out Suggested Discharge Summary Format
Thousands of positive reviews can’t be wrong
Read more or give pdfFiller a try to experience the benefits for yourself
Questions & answers
How do you do a discharge summary in simple practice?
Creating a Discharge Summary in a client's profile Navigate to the client's Overview page. Click New>Assessment. Select Discharge Summary Note.
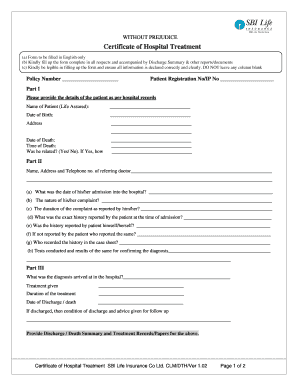
What does a discharge summary need to contain?
Most discharge letters include a section that summarises the key information of the patient's hospital stay in patient-friendly language, including investigation results, diagnoses, management and follow up. This is often given to the patient at discharge or posted out to the patient's home.
How do you write a mental health discharge summary?
DISCHARGE SUMMARY REQUIREMENTS A review of the mental health treatment. Reason for discharge. Date of discharge. Condition at discharge. Response to psychotropic medications. Collaterals notified. Recommendations for aftercare.
What should be included in a therapy discharge summary?
A discharge report written by a therapist shall include: Documentation of the patient's subjective statements, if relevant. Updated objective measures, including validated outcome surveys. Extent of progress toward each goal. which goals have been attained and which were not achieved.
How do you write a discharge summary in counseling?
What is in the discharge summary? Diagnosis at discharge. Detailed reasons for reasons for discharge (including progress toward treatment goals) Any risk factors at the time care ended. Referrals and resources of benefit to the client.
What is a discharge summary?
A discharge summary is a letter written by the doctor caring for you in hospital. It contains important information about your. hospital visit, including: • why you came into hospital.
Related templates