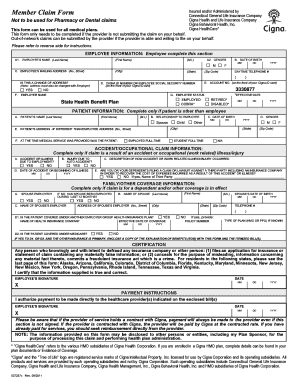
Cigna Out Of Network Claim Form
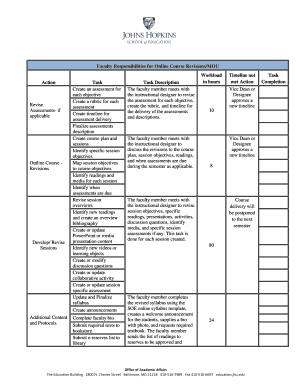
What is cigna out of network claim form?
Cigna out of network claim form is a document that allows policyholders to submit claims for medical services received from healthcare providers who do not participate in the Cigna network. It is important to fill out this form accurately and completely to ensure prompt processing of your claim.
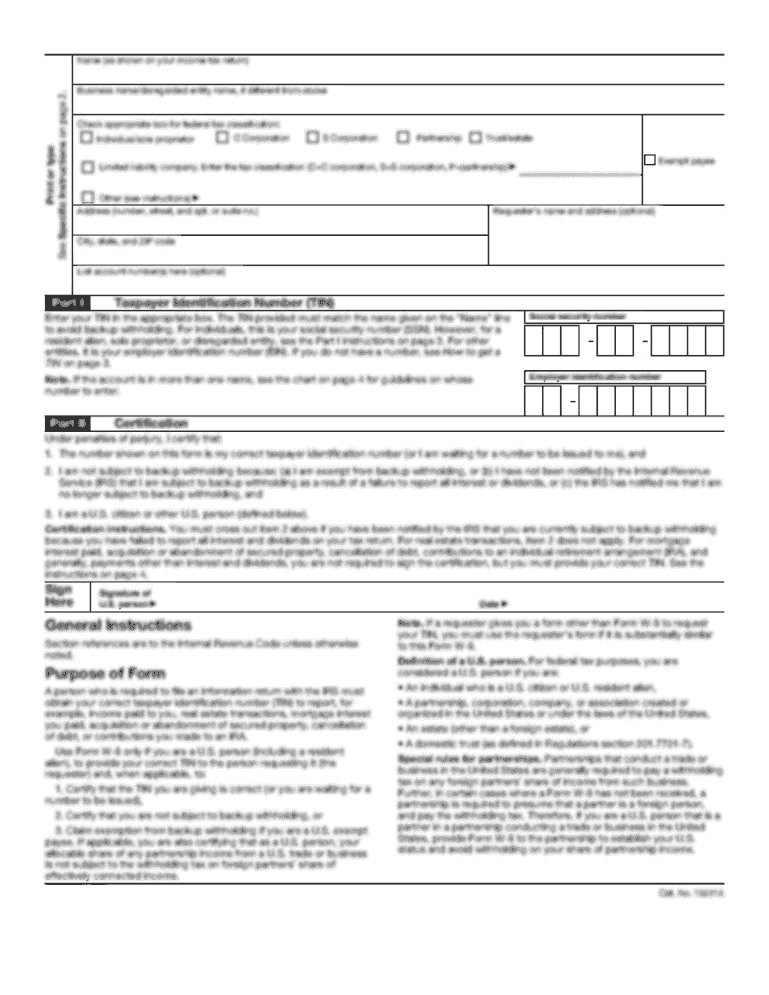
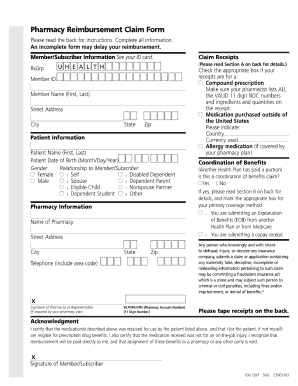
What are the types of cigna out of network claim form?
Cigna offers different types of out of network claim forms depending on the type of medical service received. Some common types of Cigna out of network claim forms include:
How to complete cigna out of network claim form
Completing a Cigna out of network claim form is simple. Here are the steps:
By using pdfFiller, you can easily create, edit, and share your Cigna out of network claim forms online. pdfFiller provides unlimited fillable templates and powerful editing tools, making it the only PDF editor you need to efficiently complete your claim forms.