Furnish Elect Notice


Users trust to manage documents on pdfFiller platform
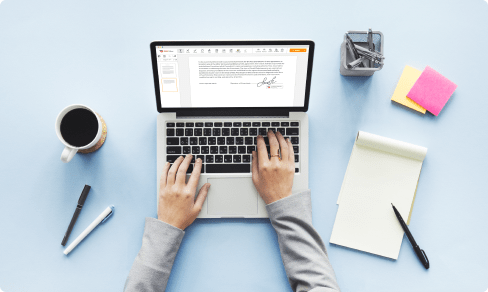
Furnish Elect Notice: make editing documents online simple
The PDF is a popular file format used for business records because you can access them from any device. It will keep the same layout no matter you open it on Mac computer or an Android smartphone.
The next point is data protection: PDF files are easy to encrypt, so they're risk-free for sharing data from person to person. Using online solutions, it is possible to get an access a viewing history to find out who had access to it before.
pdfFiller is an online document management and editing tool that lets you create, edit, sign, and share your PDFs directly from your browser. It is integrated with major Arms and allows users to sign and edit documents from other services, such as Google Docs or Office 365. Once you’ve finished changing a document, mail it to recipients to complete and get a notification when they're done.
Use editing tools such as typing text, annotating, and highlighting. Once a document is completed, download it to your device or save it to cloud storage. Add and edit visual content. Ask your recipient to fill out the fields and request an attachment if needed. Add fillable fields and send documents for signing. Change a document’s page order.
Complete any document with pdfFiller in four steps:
What our customers say about pdfFiller