Get the free medco prior authorization form pdf
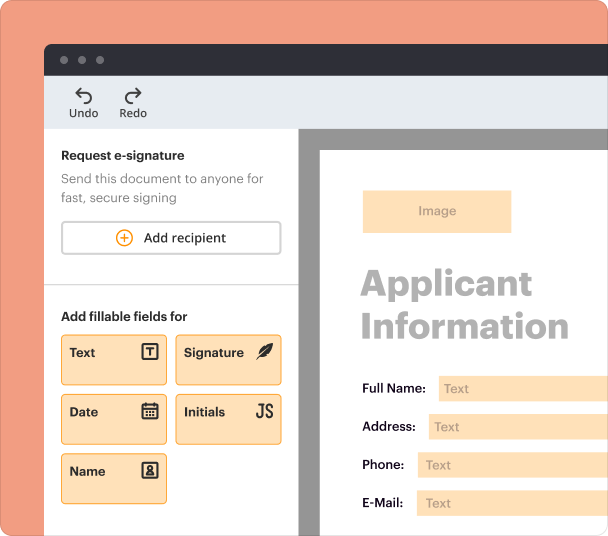
Fill out, sign, and share forms from a single PDF platform
Edit and sign in one place
Create professional forms
Simplify data collection
Manage forms centrally
Why pdfFiller is the best tool for your documents and forms
End-to-end document management
Accessible from anywhere
Secure and compliant
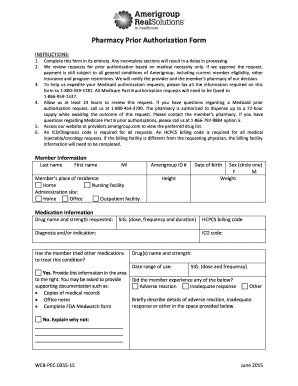
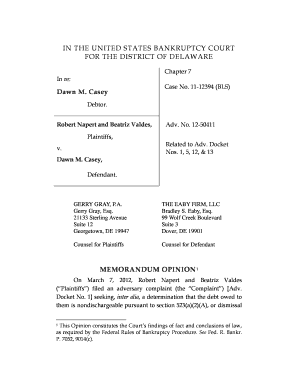
Medco Prior Authorization Form Guide
Filling out a Medco prior authorization form is essential for securing necessary medications. This guide will provide a thorough overview, from understanding the process to completing the form accurately.
What is the Medco prior authorization process?
Prior authorization is a requirement that ensures insurance covers specific medications before treatment begins. It's a critical step in medication management that involves patients, prescribers, and insurance providers.
-
Patients must be informed and involved in the prior authorization process for their prescribed treatments.
-
Prescribers are responsible for submitting the form to initiate the authorization based on the patient's medical needs.
-
Insurance providers review the authorization requests to determine coverage based on medical necessity and guidelines.
Delays can occur in the authorization process due to missing information or discrepancies. Common reasons for authorization denial include lack of medical necessity or patient eligibility issues.
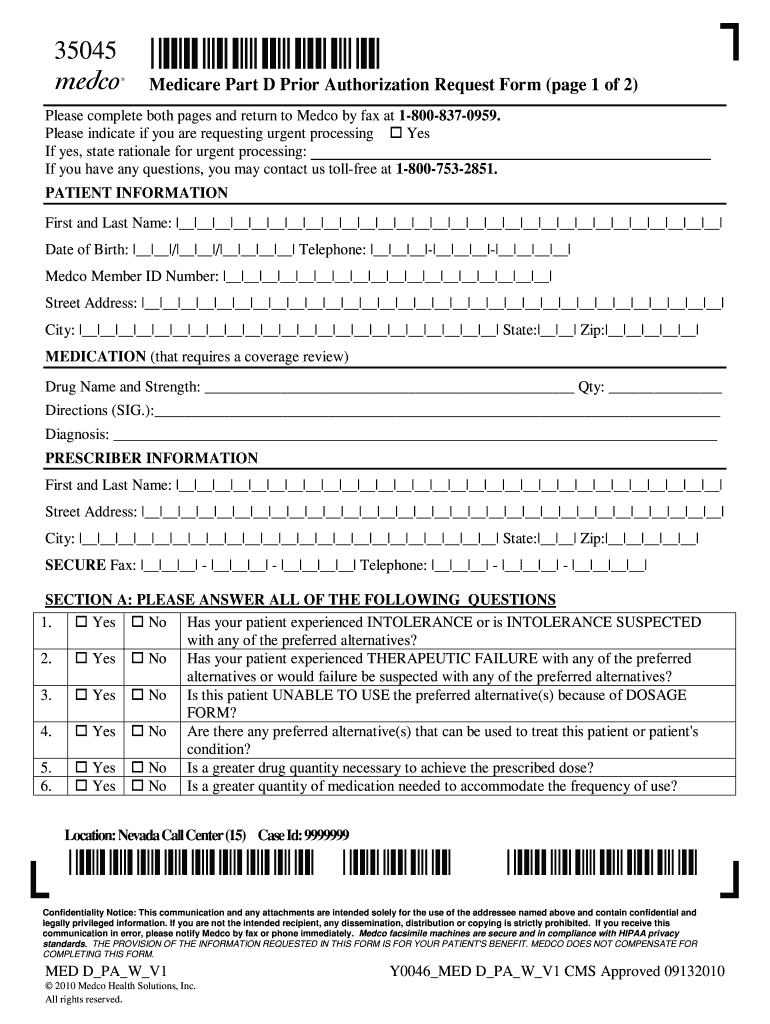
How to navigate the Medco prior authorization request form?
Understanding each section of the Medco Prior Authorization Form is essential for correct submission. This ensures that all necessary information is accurately captured.
-
Accurate patient details are critical as they verify eligibility for coverage.
-
Include the drug name, dosage, and treatment directions to ensure compliance with treatment protocols.
-
Provide details such as the prescriber's contact information and credentials, which facilitate quicker processing.
What are the steps to complete the authorization form?
Filling out the request form accurately involves several crucial steps. Follow these instructions to enhance processing efficiency.
-
Double-check all entries to avoid rejections based on simple errors.
-
If applicable, mark the request as urgent and provide a valid rationale for quicker approval.
-
Verify that prescriber and patient contact information are accurate to facilitate communication.
How to review the form submission process?
Once the Medco form is completed, submitting it correctly is paramount. This involves adhering to specific guidelines for ensuring it reaches the right department.
-
Tutoring to send the completed Medco form via fax to the designated department for processing.
-
Maintain a record of the fax confirmation to follow up on the status of the authorization.
-
Ensure confidentiality in all submissions by understanding the implications of HIPAA guidelines.
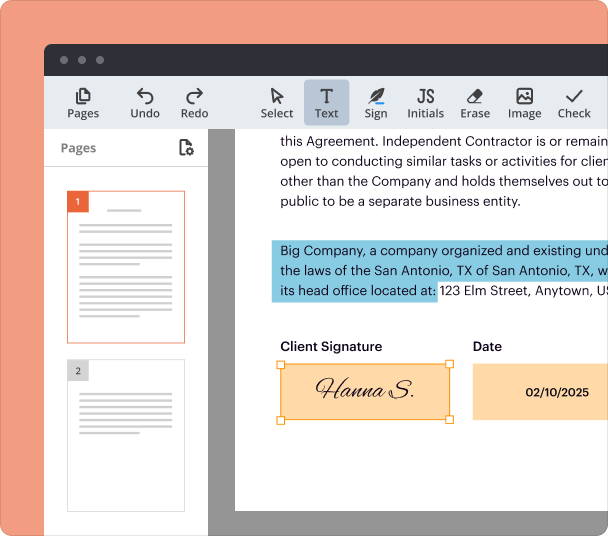
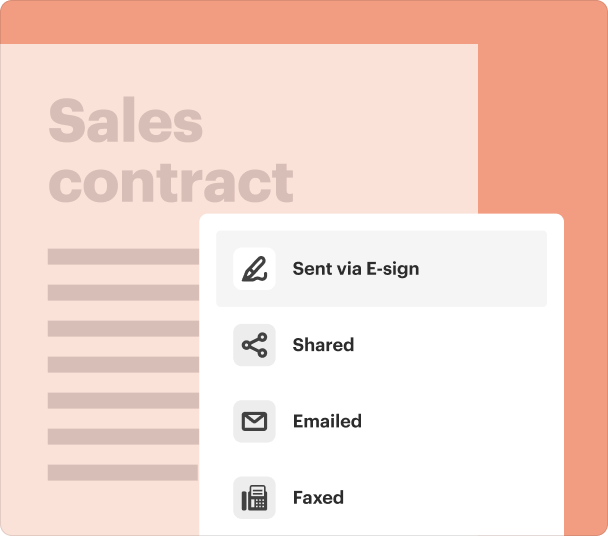
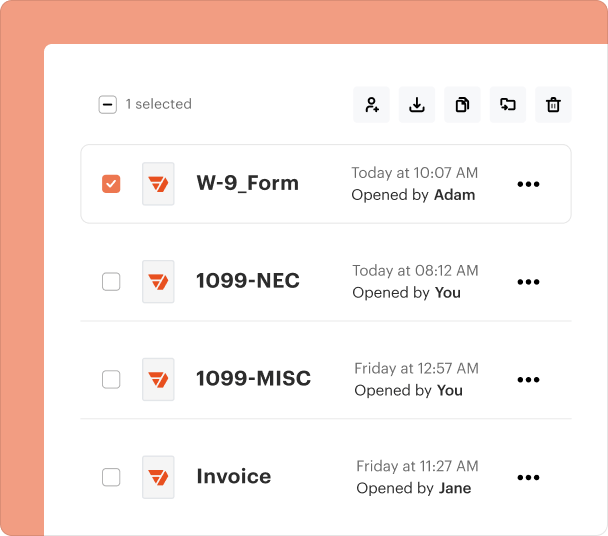
How to utilize PDFfiller’s tools for Medco form management?
PDFfiller offers a robust platform for managing the Medco Prior Authorization Form. Users can easily edit, fill out, and e-sign documents.
-
Use PDFfiller’s intuitive interface to adjust the form as needed, ensuring all fields are completed correctly.
-
Utilizing eSigning functionality speeds up the process by eliminating the need for physical signatures.
-
PDFfiller allows users to share documents with prescribers and team members for better cooperation.
What are related forms and resources?
Understanding other related documents can enhance your approach to comprehensive submissions. It’s beneficial to know what additional forms may be required.
-
Research other forms necessary for a complete submission to your insurance provider.
-
Explore links to articles or websites that explain the complexities of the prior authorization process.
-
Review differences among other insurance forms to identify unique requirements.
Frequently Asked Questions about Medco Prior Authorization Form
What should I do if my medication is denied?
If your medication is denied, contact your prescriber to discuss potential alternatives or to appeal the decision. Gathering additional supporting documents can also improve the chances of approval.
How long does the prior authorization process take?
The prior authorization process can take anywhere from a few days to a couple of weeks. Factors affecting the timeline include the complexity of the case and how quickly necessary information is provided.
Can I expedite my authorization request?
Yes, you can request urgent processing if your situation requires immediate attention. Be prepared to provide a clear justification for the urgency.
Are there exemptions to prior authorization?
Certain medications may be exempt from prior authorization requirements based on the insurance policy. It's important to check with your provider for specific details.
What if I need help filling out the form?
If you need assistance, consider reaching out to your prescriber’s office or utilizing resources available on platforms like PDFfiller that offer guides and support.
pdfFiller scores top ratings on review platforms