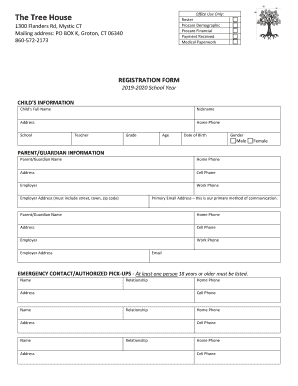
Get the free CIGNA HealthCare Prior Authorization Form
Show details
This form is used to request prior authorization for the medication Selzentry, specifically for patients diagnosed with CCR5-tropic HIV-1. It collects detailed provider and patient information, and
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign cigna healthcare prior authorization

Edit your cigna healthcare prior authorization form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your cigna healthcare prior authorization form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing cigna healthcare prior authorization online
Follow the steps down below to benefit from the PDF editor's expertise:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit cigna healthcare prior authorization. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out cigna healthcare prior authorization

How to fill out CIGNA HealthCare Prior Authorization Form
01
Obtain the CIGNA HealthCare Prior Authorization Form from the CIGNA website or your healthcare provider.
02
Fill in the patient's information, including name, date of birth, and CIGNA ID number.
03
Provide details about the requesting healthcare provider, including their name, contact information, and NPI number.
04
Indicate the specific procedure, service, or medication for which prior authorization is being requested.
05
Include relevant clinical information and medical necessity documentation to support the request.
06
Sign and date the form to certify that the information is accurate to the best of your knowledge.
07
Submit the completed form via the specified method, which may include faxing or submitting it online through the CIGNA portal.
08
Keep a copy of the submitted form for your records.
Who needs CIGNA HealthCare Prior Authorization Form?
01
Patients who require specific medical services, procedures, or medications covered by CIGNA HealthCare.
02
Healthcare providers seeking approval from CIGNA for services or treatments that may need verification of medical necessity.
03
Pharmacies that need prior authorization for certain prescriptions under CIGNA's insurance plans.
Fill
form
: Try Risk Free






People Also Ask about
How long does a prior authorization take with Cigna?
Typically, within 5-10 business days of receiving the prior authorization request, your insurance company will either: Approve your request. Deny your request.
How can I speed up my prior authorization?
Use prescribing software that offers Advanced Prior Authorization (aka Electronic Prior Authorization). The software calls out to a 3rd party who returns the exact questions the payer wants answered before approval. Approval times are drastically shorter and approval rates are way, way higher.
How long does prior authorization take for Cigna?
Typically, within 5-10 business days of receiving the prior authorization request, your insurance company will either: Approve your request. Deny your request.
How do I get a prior authorization form from Cigna?
If you are unable to use electronic prior authorization, you can call us at 1 (800) 882-4462 to submit a prior authorization request.
Is Cigna removing prior authorization?
Cigna Healthcare also recently announced plans to remove prior authorization from 25% of medical services in their commercial plans, bringing the total number of prior authorization removals to more than 1,100 since 2020.
Can I submit a prior authorization for myself?
Sometimes, your health care provider will start and coordinate the prior authorization process for you. However, you may be responsible for getting the prior authorization yourself.
How long should I wait for a prior authorization?
Typical Time Frames for Prior Authorization Normal Requests: For most medicines, getting approval can take from one to three days after sending the request. Emergency Requests: If the medicine is urgently needed, insurance companies might speed things up and decide within a day.
What does a prior authorization representative do at Cigna?
The Prior Authorization Representative at Cigna plays a vital role in the Coverage Review Department, focusing on determining the coverage eligibility of prescribed procedures, services, or medications for members.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is CIGNA HealthCare Prior Authorization Form?
The CIGNA HealthCare Prior Authorization Form is a document that healthcare providers use to obtain approval from CIGNA before providing certain medical services or treatments to ensure they are covered under a patient's insurance plan.
Who is required to file CIGNA HealthCare Prior Authorization Form?
Healthcare providers who are seeking approval for specific procedures, medications, or treatments for their patients that require prior authorization under CIGNA HealthCare policies must file this form.
How to fill out CIGNA HealthCare Prior Authorization Form?
To fill out the CIGNA HealthCare Prior Authorization Form, the healthcare provider must provide patient information, the nature of the requested service or treatment, clinical information supporting the request, and any relevant codes or documentation required by CIGNA.
What is the purpose of CIGNA HealthCare Prior Authorization Form?
The purpose of the CIGNA HealthCare Prior Authorization Form is to ensure that requested medical services are medically necessary, appropriate, and covered under a patient's health insurance plan before they are provided.
What information must be reported on CIGNA HealthCare Prior Authorization Form?
The CIGNA HealthCare Prior Authorization Form must report information such as patient demographics, provider details, specific service or treatment requested, medical necessity justification, and any relevant clinical information or history.
Fill out your cigna healthcare prior authorization online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Cigna Healthcare Prior Authorization is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.