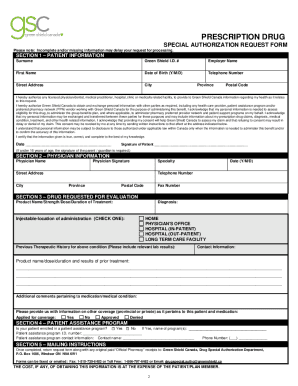
Canada GSC Prescription Drug Special Authorization Request 2008 free printable template
Show details
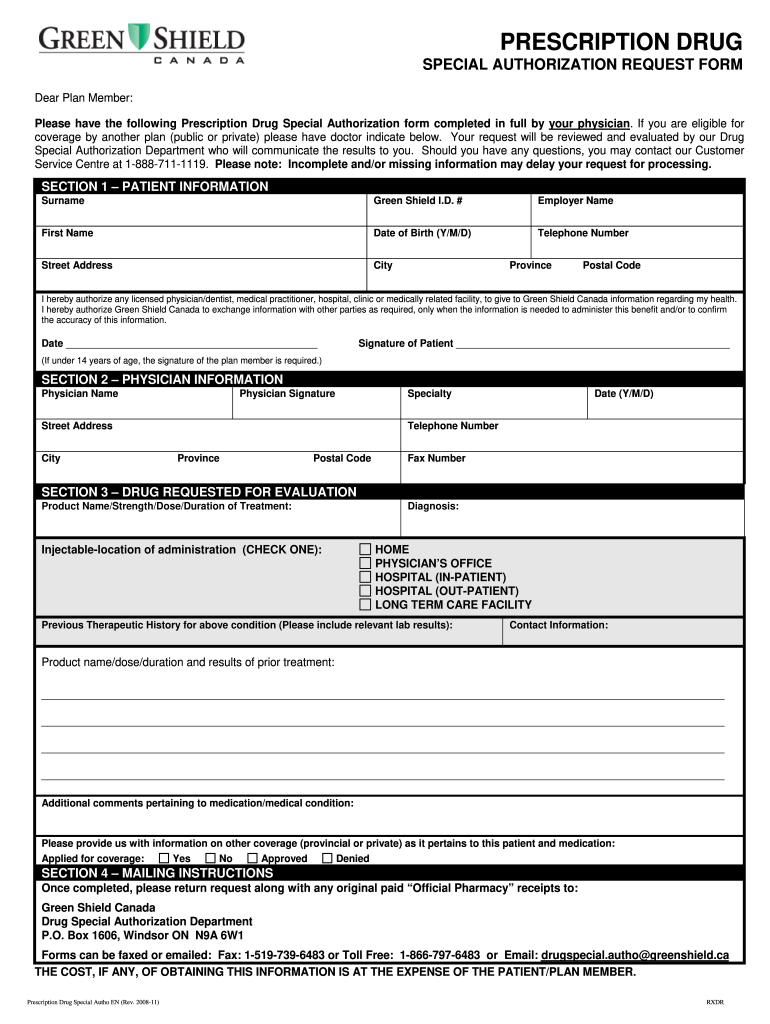
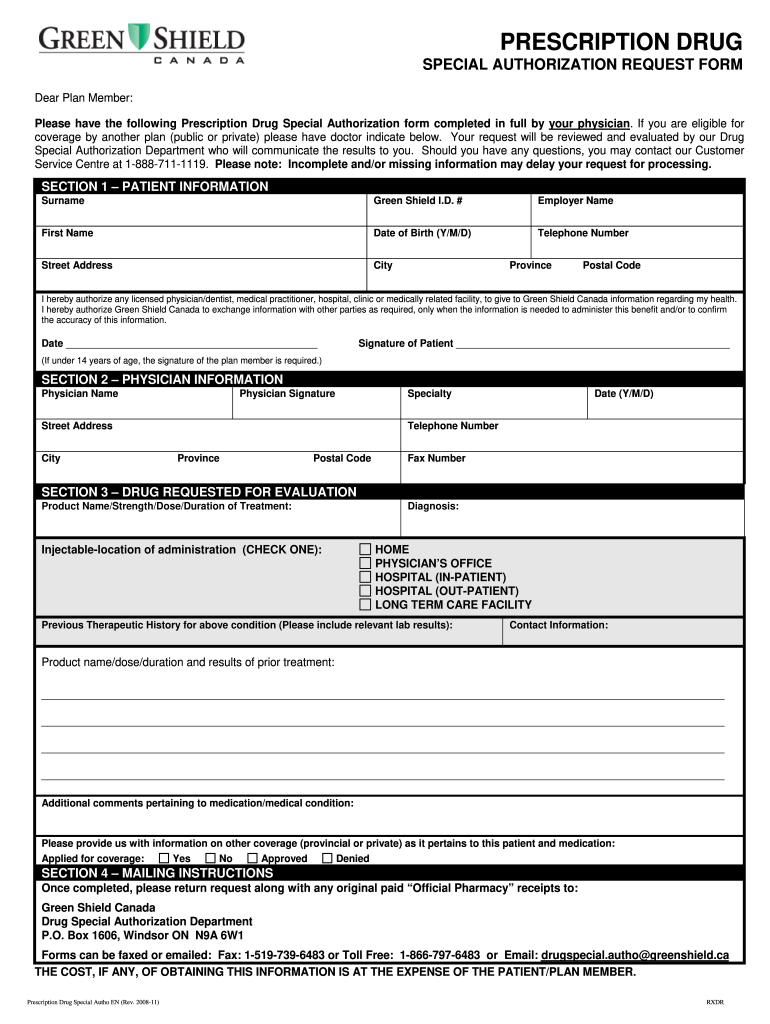
PRESCRIPTION DRUG
SPECIAL AUTHORIZATION REQUEST FORM
Dear Plan Member:
Please have the following Prescription Drug Special Authorization form completed in full by your physician. If you are eligible
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign Canada GSC Prescription Drug Special Authorization
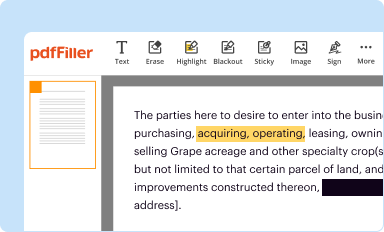
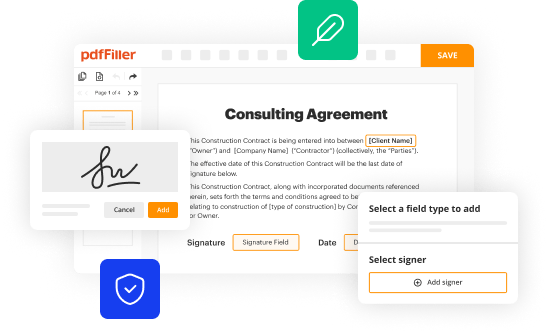
Edit your Canada GSC Prescription Drug Special Authorization form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
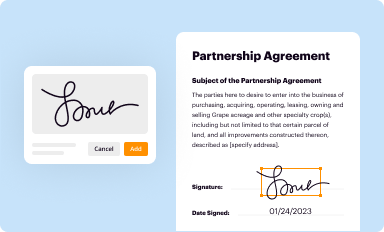
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
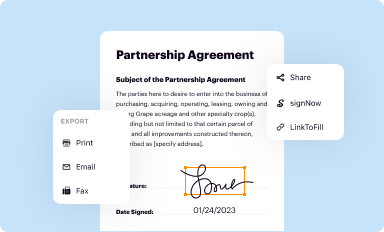
Share your form instantly
Email, fax, or share your Canada GSC Prescription Drug Special Authorization form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit Canada GSC Prescription Drug Special Authorization online
Follow the guidelines below to benefit from the PDF editor's expertise:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit Canada GSC Prescription Drug Special Authorization. Add and change text, add new objects, move pages, add watermarks and page numbers, and more. Then click Done when you're done editing and go to the Documents tab to merge or split the file. If you want to lock or unlock the file, click the lock or unlock button.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
It's easier to work with documents with pdfFiller than you could have ever thought. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
Canada GSC Prescription Drug Special Authorization Request Form Versions
Version
Form Popularity
Fillable & printabley
How to fill out Canada GSC Prescription Drug Special Authorization
How to fill out Canada GSC Prescription Drug Special Authorization Request
01
Obtain the Canada GSC Prescription Drug Special Authorization Request form from your healthcare provider or the GSC website.
02
Fill in your personal details such as name, address, and policy number at the top of the form.
03
Provide the patient's information if different from the policy holder.
04
Indicate the prescribed medication(s) that require special authorization.
05
Include the medical diagnosis and justification for the need of the prescribed medication.
06
Ensure that your healthcare provider completes the provider information section including their signature.
07
Review the form for completeness and accuracy before submission.
08
Submit the completed form to GSC via the indicated method (fax, email, or mail).
Who needs Canada GSC Prescription Drug Special Authorization Request?
01
Individuals who have been prescribed medication that is not typically covered under their insurance plan and require prior approval for coverage.
02
Patients with specific medical conditions that necessitate the use of specialized or experimental drugs.
03
Healthcare providers seeking authorization on behalf of their patients to ensure necessary medications are covered.
Fill
form
: Try Risk Free






People Also Ask about
Does Alberta have a drug plan?
Albertans can access prescription drug coverage through a number of programs. Supports for individuals and families to pay for basic expenses like food, clothing and shelter. Learn about Non-Group Coverage for supplementary health benefits, eligibility, benefits covered and premiums.
What is prior authorization in pharmacy?
Prior authorization requires the prescriber to receive pre-approval for prescribing a particular drug in order for that medication to qualify for coverage under the terms of the pharmacy benefit plan.
How does pre-authorization work?
A pre-authorization is a restriction placed on certain medications, tests, or health services by your insurance company that requires your doctor to first check and be granted permission before your plan will cover the item.
What is covered by Green Shield?
Popular Green Shield Canada Benefits All packages include emergency care, vision care, therapists, and specialists. Green Shield offers 24/7 support for insurance and legal questions through the Green Shield CA login. Their mobile app lets customers file claims and check claim status easily.
What is an example of prior authorization?
For example, your health plan may require prior authorization for an MRI, so that they can make sure that a lower-cost x-ray wouldn't be sufficient. The service isn't being duplicated: This is a concern when multiple specialists are involved in your care.
What is special Authorization Newfoundland and Labrador Prescription Drug Program?
Special Authorization is a process whereby beneficiaries of the Newfoundland and Labrador Prescription Drug Program (NLPDP) may obtain drug products not offered as open benefits under the Prescription Drug Program.
Why are prescription drugs not covered by insurance?
That means sometimes we may not cover a drug your doctor has prescribed. It might be because it's a new drug that doesn't yet have a proven safety record. Or, there might be a less expensive drug that works just as well.
What does it mean when a drug needs prior authorization?
What is prior authorization? This means we need to review some medications before your plan will cover them. We want to know if the medication is medically necessary and appropriate for your situation. If you don't get prior authorization, a medication may cost you more, or we may not cover it.
What is the Alberta special Authorization program?
Special authorization benefits Special authorization is a mechanism to provide access to certain drugs ing to defined clinical criteria. Special authorization request forms are completed by physicians and reviewed by clinical pharmacists. Prior approval must be granted to ensure coverage by special authorization.
What is the meaning of prior authorization?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
Does green shield cover out of province?
Out of province hospital and medical services coverage is provided by Allianz Global Assistance, through Green Shield Canada, to eligible employees and retirees who meet the Canadian residency requirements.
How does a prior authorization work?
Prior authorization (also called “preauthorization” and “precertification”) refers to a requirement by health plans for patients to obtain approval of a health care service or medication before the care is provided. This allows the plan to evaluate whether care is medically necessary and otherwise covered.
Which procedure is most likely to need a prior authorization?
In most cases, the services that require this approval are those deemed expensive or high risk. For many carriers, the following services require prior approval: Diagnostic imaging such as MRIs, CTs and PET scans. Durable medical equipment such as wheelchairs, at-home oxygen and patient lifts.
Why is it called prior authorization?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
What is meant by prior authorization?
A decision by your health insurer or plan that a health care service, treatment plan, prescription drug or durable medical equipment is medically necessary. Sometimes called prior authorization, prior approval or precertification.
Does greenshield cover medication?
Green S GSC Health Assist ZONE plans offer varying levels of health, dental, drug and travel coverage in a selection of bundled plans – at competitive prices.
What is a special authorization form?
Special Authorization and Prior Authorization are interchangeable terms we use to describe a pre-approval process that helps us determine if certain prescription drugs will be reimbursed under your benefit plan. Most drugs that require prior authorization are considered high-cost specialty drugs.
Does Green Shield do direct billing?
You're all-in on direct billing. We're here to help you spread the word. Our plug and play marketing toolkit sets you up to promote direct billing via your website, social media pages, waiting room and more.
Is prior authorization the same as a prescription?
Ask your health care provider if a prescription or medical treatment is going to require prior authorization so they can start the process immediately. This is not the same as if you need additional treatments or prescriptions after your initial visit.
Our user reviews speak for themselves
Read more or give pdfFiller a try to experience the benefits for yourself
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my Canada GSC Prescription Drug Special Authorization directly from Gmail?
The pdfFiller Gmail add-on lets you create, modify, fill out, and sign Canada GSC Prescription Drug Special Authorization and other documents directly in your email. Click here to get pdfFiller for Gmail. Eliminate tedious procedures and handle papers and eSignatures easily.
How do I execute Canada GSC Prescription Drug Special Authorization online?
Easy online Canada GSC Prescription Drug Special Authorization completion using pdfFiller. Also, it allows you to legally eSign your form and change original PDF material. Create a free account and manage documents online.
How do I edit Canada GSC Prescription Drug Special Authorization straight from my smartphone?
The easiest way to edit documents on a mobile device is using pdfFiller’s mobile-native apps for iOS and Android. You can download those from the Apple Store and Google Play, respectively. You can learn more about the apps here. Install and log in to the application to start editing Canada GSC Prescription Drug Special Authorization.
What is Canada GSC Prescription Drug Special Authorization Request?
The Canada GSC Prescription Drug Special Authorization Request is a process that allows healthcare providers to request coverage for specific medications that are not typically covered under a patient's drug plan. This process helps ensure that individuals have access to necessary treatments when standard coverage limits are not applicable.
Who is required to file Canada GSC Prescription Drug Special Authorization Request?
Healthcare providers, such as doctors or pharmacists, are required to file the Canada GSC Prescription Drug Special Authorization Request on behalf of their patients who need prior approval for certain prescription drugs.
How to fill out Canada GSC Prescription Drug Special Authorization Request?
To fill out the Canada GSC Prescription Drug Special Authorization Request, the healthcare provider must complete a standardized form that includes patient information, prescription details, medical history, and justification for the need for the medication based on the patient's condition.
What is the purpose of Canada GSC Prescription Drug Special Authorization Request?
The purpose of the Canada GSC Prescription Drug Special Authorization Request is to evaluate and determine whether a specific drug should be covered under a patient's insurance plan, ensuring that only necessary and appropriate medications are authorized for reimbursement.
What information must be reported on Canada GSC Prescription Drug Special Authorization Request?
The information that must be reported includes the patient's personal and insurance details, the prescribing physician's information, the specific drug requested, an explanation of the medical necessity, related diagnoses, and any relevant treatment history.
Fill out your Canada GSC Prescription Drug Special Authorization online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Canada GSC Prescription Drug Special Authorization is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.