Discharge Instruction Sheet Turp Patient 2004-2026 free printable template
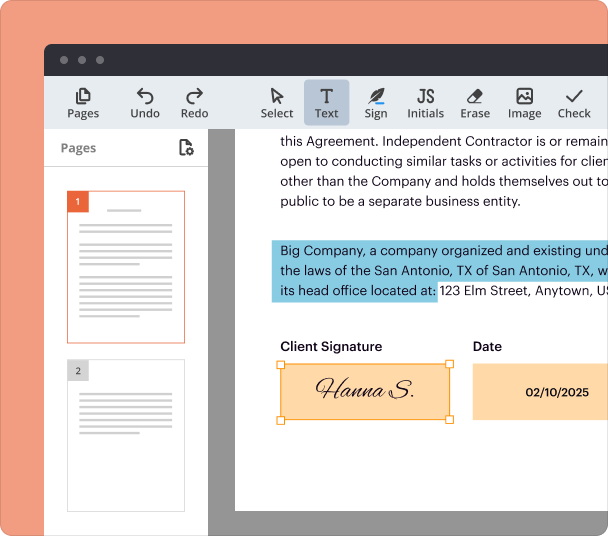
Fill out, sign, and share forms from a single PDF platform
Edit and sign in one place
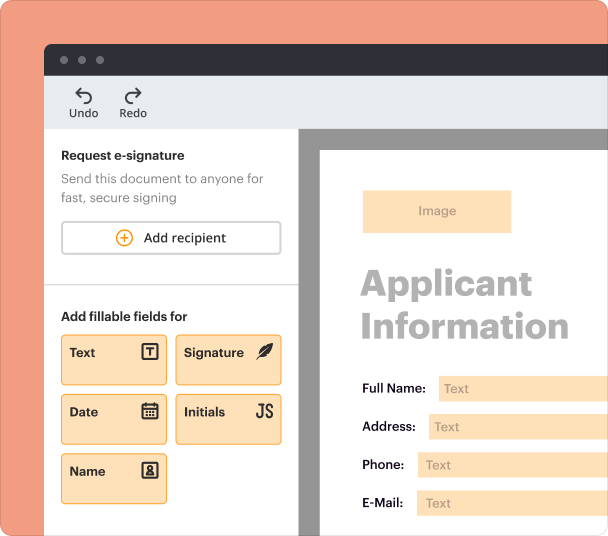
Create professional forms
Simplify data collection
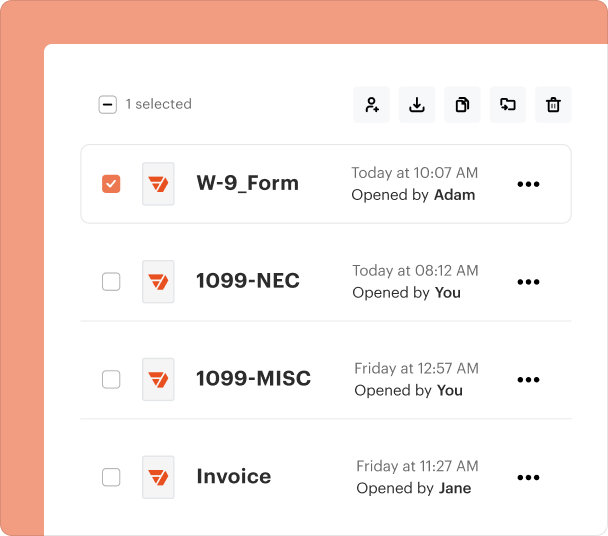
Manage forms centrally
Why pdfFiller is the best tool for your documents and forms
End-to-end document management
Accessible from anywhere
Secure and compliant
Comprehensive Guide to the Discharge Instruction Sheet for TURP Patients
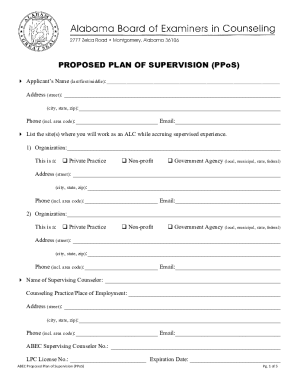
Overview of the Discharge Instruction Sheet for TURP
The discharge instruction sheet for Transurethral Resection of the Prostate (TURP) serves as a vital document that outlines the necessary post-operative care for patients. It includes a range of instructions specifically designed to ensure a safe recovery, highlighting activity limitations, medication guidelines, dietary recommendations, and important follow-up actions.
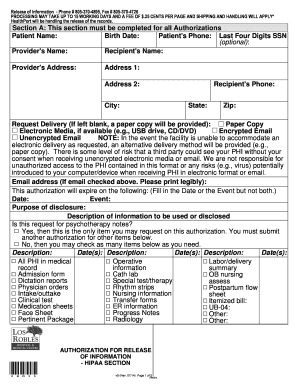
Essential Components of the Discharge Instruction Sheet
The instruction sheet typically includes several key elements to facilitate recovery: instructions regarding activity restrictions, guidelines for medication management, dietary suggestions, recommended exercises, and indications when to seek medical attention. Emphasis on patient education ensures that individuals can manage their recuperation effectively.
Important Activity Restrictions Post-TURP
Following TURP, patients are generally advised to avoid heavy lifting, long periods of sitting, and vigorous activities such as driving or sports for at least three weeks. Short walks are encouraged to promote circulation, but any strenuous exercise should be postponed until cleared by a physician.
Dietary Recommendations for TURP Patients
Diet plays an essential role in recovery. Patients are typically advised to maintain a balanced diet that is high in fiber to prevent constipation, which can strain the surgical site. Adequate hydration is crucial, with an emphasis on drinking sufficient fluids daily, largely around twelve glasses of water, to promote urinary health.
When to Contact Your Doctor
It is vital for patients to be aware of when to seek medical advice post-procedure. They should contact their healthcare provider if they experience increased bleeding, difficulty with urination, or have any concerns that may arise during their recovery. Early intervention can be key to addressing complications.
Documentation and Signatures
The discharge instruction sheet should be signed by both the discharging physician and the patient or responsible person, indicating that the patient has received and understood the instructions. This ensures clarity and accountability for both parties, establishing a clear line of communication regarding post-operative care.
Benefits of Properly Following Discharge Instructions
Adhering to the discharge instructions has numerous benefits, including a smoother recovery, reduced risk of complications, and improved overall health outcomes. By following the outlined activities, diet, and medication protocols, patients set themselves up for a more effective healing process and a return to their daily activities.
Frequently Asked Questions about hospital discharge papers pdf form
What should I do if I forgot to follow an instruction after discharge?
If you missed any instructions, it is important to contact your healthcare provider for guidance on how to address the situation and ensure your recovery remains on track.
Is it normal to experience discomfort after TURP?
Some discomfort is expected after the procedure. However, if pain becomes severe or is accompanied by unusual symptoms, you should consult your doctor.
pdfFiller scores top ratings on review platforms