Get the free Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company
Show details
Appeal Information Packet and Other Important Disclosure Information Arizona Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company PLEASE READ THIS NOTICE CAREFULLY AND KEEP IT FOR FUTURE REFERENCE. IT CONTAINS IMPORTANT INFORMATION ABOUT HOW TO APPEAL DECISIONS WE MAKE ABOUT YOUR HEALTH CARE COVERAGE. Getting Information about the Health Care Appeals Process Decisions You Can Appeal You can appeal the following de...
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign health care insurer appeals
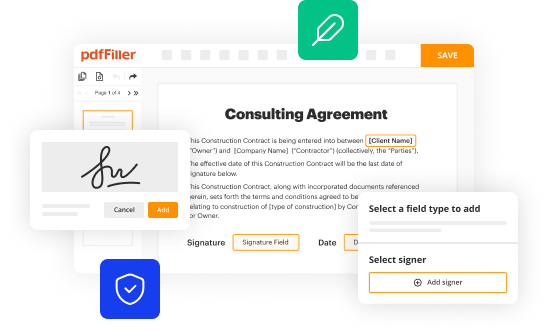
Edit your health care insurer appeals form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your health care insurer appeals form via URL. You can also download, print, or export forms to your preferred cloud storage service.
Editing health care insurer appeals online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Check your account. In case you're new, it's time to start your free trial.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit health care insurer appeals. Rearrange and rotate pages, insert new and alter existing texts, add new objects, and take advantage of other helpful tools. Click Done to apply changes and return to your Dashboard. Go to the Documents tab to access merging, splitting, locking, or unlocking functions.
4
Get your file. Select the name of your file in the docs list and choose your preferred exporting method. You can download it as a PDF, save it in another format, send it by email, or transfer it to the cloud.
It's easier to work with documents with pdfFiller than you can have believed. You may try it out for yourself by signing up for an account.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out health care insurer appeals
How to fill out Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company
01
Obtain the Health Care Insurer Appeals Process Information Packet from Aetna's website or customer service.
02
Carefully read the instructions provided in the packet.
03
Fill out your personal information in the designated sections including name, address, and policy number.
04
Provide details about the claim you are appealing, including dates of service and specific reasons for the appeal.
05
Attach any supporting documents such as medical records, bills, or previous correspondence with Aetna.
06
Review your completed packet to ensure all required information is included and clearly written.
07
Submit the packet via the method specified in the instructions (mail, fax, or online portal).
08
Keep a copy of the filled-out packet and any submitted documents for your records.
Who needs Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company?
01
Individuals who have had a claim denied by Aetna and wish to appeal the decision.
02
Patients seeking to reverse a coverage decision made by Aetna.
03
Health care providers representing patients in the appeals process with Aetna.
Fill
form
: Try Risk Free






People Also Ask about
How do health insurance appeals work?
Health insurance appeals are complicated. Typically, a formal appeal begins with a ``peer-to-peer'' call between the prescribing physician and a physician employed by the insurer, followed by the submission of additional documentation of medical necessity, then the wait for a response.
What is the timely filing limit for Aetna Better health of NJ appeal?
All appeals go through our Utilization Management Appeal process. You can ask for an appeal verbally or in writing. You have 60 calendar days from the date on your Notice of Adverse Benefit Determination to ask for an appeal.
How long does Aetna take to process an appeal?
Level I Appeal A Level I appeal is your initial appeal, and you must submit it within 180 calendar days from the time you receive the notice of an adverse benefit determination on the Explanation of Benefits. Aetna will communicate the Level I appeal decision in writing within 30 days of receiving the appeal.
How to appeal an Aetna insurance denial?
In either case, if you do not agree with our decision, you can ask for a second review. You have 60 days from the date that you get the appeal decision letter to let us know. You can call Member Services at the phone number listed on your member ID card, or write to us.
What is the timeframe for Aetna appeal?
You can file an appeal within 180 days of receiving a Notice of Action. The Appeals and Grievance Manager will send an acknowledgment letter within five business days. The letter will summarize the appeal and include instructions on how to: Revise the appeal within the time frame specified in the acknowledgment letter.
What is the timely filing limit for Aetna Better health New Jersey appeal?
Both in-network and out-of-network providers have the right to appeal our claims determinations within 60 calendar days of receipt of the claim denial.
How do I appeal a medicare denial at Aetna?
You can file your standard or expedited appeal using one of the four methods below: Online option: Appeal a denial online. Phone option: 1-866-235-5660 (TTY: 711), 7 days a week, 24 hours a day. Or, download, print, and send completed forms by fax or mail:
What is Aetna's timely filing limit for appeals?
Timeframes for reconsiderations and appeals. Within 180 calendar days of the initial claim decision. Within 45 business days of receiving the request, depending on the matter in question, and if review by a specialty unit is needed. Submit online and check the status through your secure provider website.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company?
The Health Care Insurer Appeals Process Information Packet is a document provided by Aetna Life Insurance Company that outlines the procedures and guidelines for appealing decisions made regarding health care claims and services.
Who is required to file Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company?
Patients or policyholders who believe that a claim has been denied improperly or who disagree with an insurance decision related to their health care services are required to file this packet.
How to fill out Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company?
To fill out the packet, individuals should carefully read the instructions provided, gather necessary documentation, complete all required fields accurately, and submit it along with any supporting evidence related to their claim.
What is the purpose of Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company?
The purpose of the packet is to guide patients through the appeals process, ensuring that their concerns regarding denied claims are addressed and reviewed by Aetna Life Insurance Company.
What information must be reported on Health Care Insurer Appeals Process Information Packet - Aetna Life Insurance Company?
The information that must be reported includes the patient's personal details, policy information, details of the denied claim, reasons for the appeal, and any relevant medical documentation that supports the case.
Fill out your health care insurer appeals online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Health Care Insurer Appeals is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.