Get the free Health Care Insurer Appeals Process Information Packet - Aetna Health Inc./Corporation
Show details
This document provides essential information regarding the appeals process for health care coverage decisions made by Aetna, detailing how members can appeal decisions about their health care services,
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign health care insurer appeals
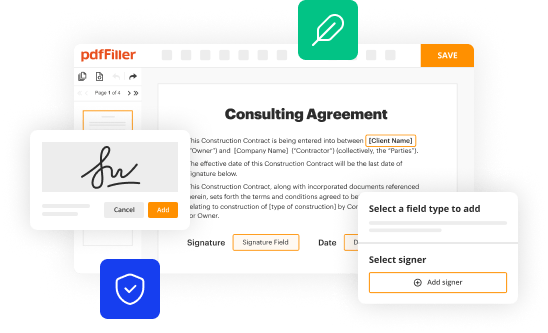
Edit your health care insurer appeals form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
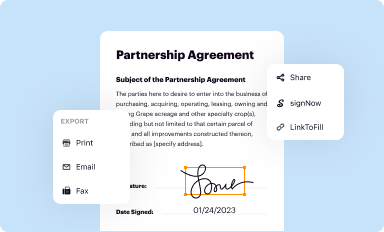
Share your form instantly
Email, fax, or share your health care insurer appeals form via URL. You can also download, print, or export forms to your preferred cloud storage service.
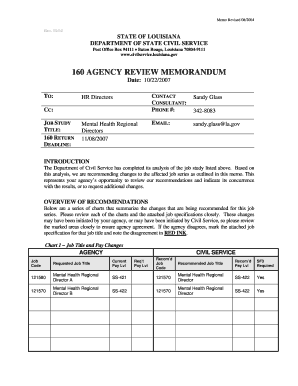
Editing health care insurer appeals online
Here are the steps you need to follow to get started with our professional PDF editor:
1
Log in to your account. Click Start Free Trial and sign up a profile if you don't have one yet.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit health care insurer appeals. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Save your file. Select it from your records list. Then, click the right toolbar and select one of the various exporting options: save in numerous formats, download as PDF, email, or cloud.
With pdfFiller, it's always easy to deal with documents.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out health care insurer appeals
How to fill out Health Care Insurer Appeals Process Information Packet - Aetna Health Inc./Corporation
01
Obtain the Health Care Insurer Appeals Process Information Packet from Aetna's website or customer service.
02
Read the entire document carefully to understand the appeals process.
03
Fill out the personal information section with your name, address, and policy details.
04
Provide details about the claim you are appealing, including claim number and date of service.
05
Explain the reason for your appeal clearly and concisely.
06
Attach any supporting documents, such as medical records or bills, that support your case.
07
Review the completed packet for accuracy and ensure all required fields are filled out.
08
Submit the packet via the method specified in the document, such as mail or online submission.
Who needs Health Care Insurer Appeals Process Information Packet - Aetna Health Inc./Corporation?
01
Individuals whose health insurance claims have been denied or partially paid by Aetna.
02
Patients who believe their health care services should be covered under their policy.
03
Representatives or family members of insured individuals assisting in the appeal process.
Fill
form
: Try Risk Free






People Also Ask about
What is the phone number for Banner Aetna member services?
For more help understanding what you need prior authorization for, call the Member Services number on your member ID card, 1-833-570-6670 (TTY: 711). We're available between 8 AM and 8 PM, 7 days a week. Are you happy with your Aetna plan? If so, consider referring a friend or family member.
What number is 1 800 624 0756?
National Medicare Dentist Line: Have a question? Call the National Medicare Dentist Line at 1-800-624-0756.
How do health insurance appeals work?
You must file your internal appeal within 180 days (6 months) of receiving notice that your claim was denied. If you have an urgent health situation, you can ask for an external review at the same time as your internal appeal. If your insurance company still denies your claim, you can file for an external review.
What is the timely filing limit for Aetna appeals?
You can file an appeal within 180 days of receiving a Notice of Action. The Appeals and Grievance Manager will send an acknowledgment letter within five business days. The letter will summarize the appeal and include instructions on how to: Revise the appeal within the time frame specified in the acknowledgment letter.
Does Aetna call you?
General Questions. If you'd like more information about BannerlAetna or have a question, just call our toll-free number at 1-800-381-6789.
What is the number for Aetna 1 800 624 0756?
Have dispute process questions? Or contact our Provider Service Center (staffed 8 AM to 5 PM local time): 1-800-624-0756 (TTY: 711) for HMO-based benefit plans. 1-888-632-3862 (TTY: 711) for indemnity and PPO-based benefit plans.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is Health Care Insurer Appeals Process Information Packet - Aetna Health Inc./Corporation?
The Health Care Insurer Appeals Process Information Packet is a document provided by Aetna Health Inc./Corporation that outlines the steps and procedures for consumers to appeal decisions made by the insurer regarding claims, coverage, or services.
Who is required to file Health Care Insurer Appeals Process Information Packet - Aetna Health Inc./Corporation?
Any member or insured individual who disagrees with a decision made by Aetna Health Inc./Corporation regarding their health care coverage or claim is required to file the Health Care Insurer Appeals Process Information Packet.
How to fill out Health Care Insurer Appeals Process Information Packet - Aetna Health Inc./Corporation?
To fill out the Health Care Insurer Appeals Process Information Packet, individuals must provide their personal information, details of the claim or decision being appealed, and any supporting documentation required by Aetna Health Inc./Corporation.
What is the purpose of Health Care Insurer Appeals Process Information Packet - Aetna Health Inc./Corporation?
The purpose of the Health Care Insurer Appeals Process Information Packet is to inform members of their rights and provide a structured process for challenging decisions made by the insurer regarding health care services and claims.
What information must be reported on Health Care Insurer Appeals Process Information Packet - Aetna Health Inc./Corporation?
The information required includes the member's identification details, the specifics of the claim or service involved, reasons for the appeal, as well as any relevant documents that support the appeal.
Fill out your health care insurer appeals online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Health Care Insurer Appeals is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.