NHAMCS-173 2011 free printable template
Show details
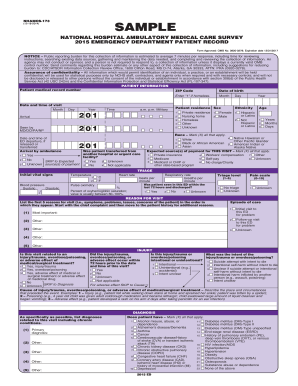
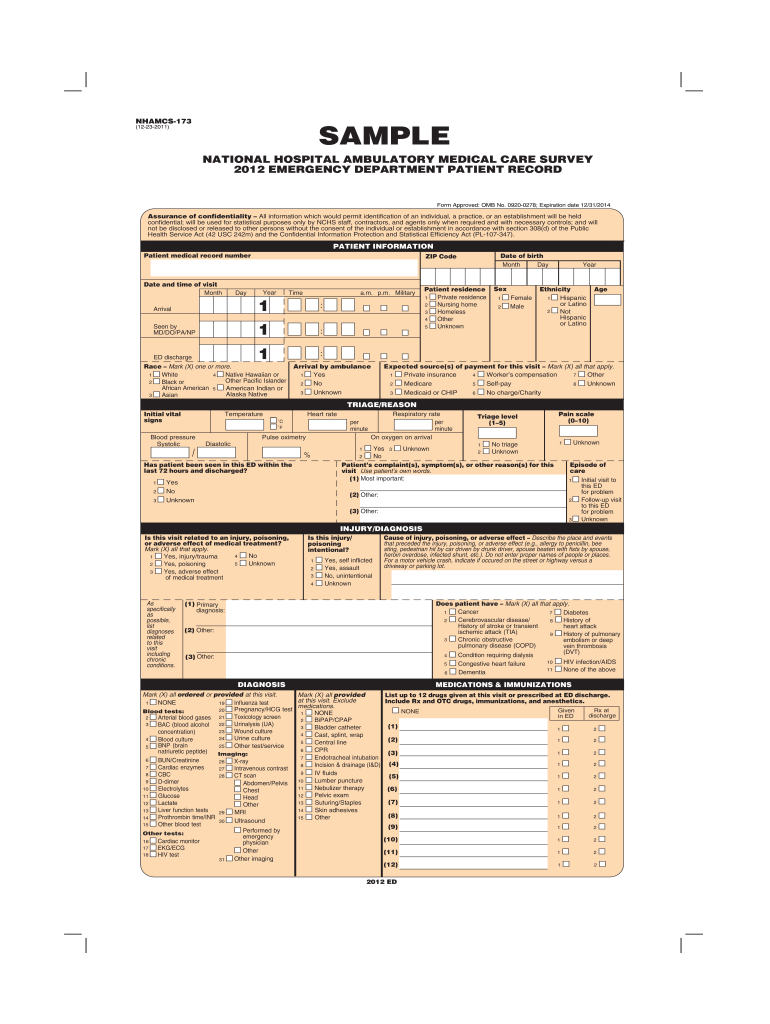
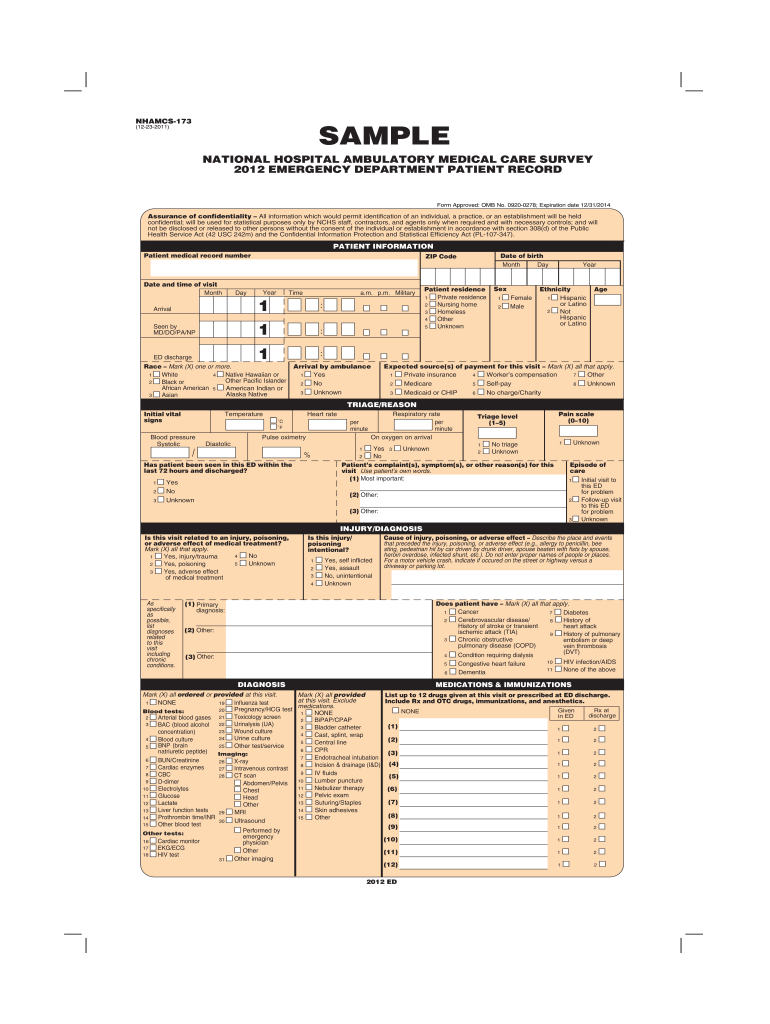
NHAMCS-173 (12-23-2011) SAMPLE NATIONAL HOSPITAL AMBULATORY MEDICAL CARE SURVEY 2012 EMERGENCY DEPARTMENT PATIENT RECORD Form Approved: OMB No. 0920-0278; Expiration date 12/31/2014 Assurance of confidentiality
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign NHAMCS-173

Edit your NHAMCS-173 form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your NHAMCS-173 form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit NHAMCS-173 online
Use the instructions below to start using our professional PDF editor:
1
Register the account. Begin by clicking Start Free Trial and create a profile if you are a new user.
2
Prepare a file. Use the Add New button. Then upload your file to the system from your device, importing it from internal mail, the cloud, or by adding its URL.
3
Edit NHAMCS-173. Add and replace text, insert new objects, rearrange pages, add watermarks and page numbers, and more. Click Done when you are finished editing and go to the Documents tab to merge, split, lock or unlock the file.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
With pdfFiller, it's always easy to deal with documents.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
NHAMCS-173 Form Versions
Version
Form Popularity
Fillable & printabley
How to fill out NHAMCS-173

How to fill out NHAMCS-173
01
Obtain the NHAMCS-173 form from the official website or request a copy.
02
Read the instructions provided with the form carefully.
03
Fill out the header section with facility information including name, address, and contact details.
04
Complete sections regarding patient demographics such as age, gender, and visit type.
05
Provide detailed information about diagnoses and procedures performed during the visit.
06
Ensure all data is accurately entered and matches the source documentation.
07
Review the form thoroughly for any errors or omissions.
08
Submit the completed form by the specified deadline.
Who needs NHAMCS-173?
01
Healthcare providers participating in the NHAMCS study.
02
Researchers needing data on emergency department visits.
03
Policy makers and public health officials for health statistics.
04
Institutions or organizations conducting health services research.
Fill
form
: Try Risk Free






People Also Ask about
What does discharged from the ER mean?
A hospital will discharge you when you no longer need to receive inpatient care and can go home. Or, a hospital will discharge you to send you to another type of facility. Many hospitals have a discharge planner. This person helps coordinate the information and care you'll need after you leave.
What must be included within a discharge summary submitted as a physician provider type?
The Joint Commission (TJC) mandates that a discharge summary be produced for every patient by the hospital provider within 30 days of discharge,4 and include (1) reason for hospitalization; (2) procedures performed; (3) care, treatment, and services provided; (4) discharge condition; (5) information provided to the
How do you write a discharge document?
6 Components of a Hospital Discharge Summary Reason for hospitalization: description of the patient's primary presenting condition; and/or. Significant findings: Procedures and treatment provided: Patient's discharge condition: Patient and family instructions (as appropriate): Attending physician's signature:
What does a discharge summary look like?
A discharge summary is a handover document that explains to any other healthcare professional why the patient was admitted, what has happened to them in hospital, and all the information that they need to pick up the care of that patient quickly and effectively.
What is included in discharge paperwork?
6 Components of a Hospital Discharge Summary Reason for hospitalization: description of the patient's primary presenting condition; and/or. Significant findings: Procedures and treatment provided: Patient's discharge condition: Patient and family instructions (as appropriate): Attending physician's signature:
How do you start a discharge letter?
Here is the ideal structure for the body of the letter in relation to medical case notes: Introduction. Body Paragraph 1 – Past medical history. Body Paragraph 2 – Hospitalisation. Body Paragraph 3 – Current Condition & Discharge Plan. Conclusion.
How do you discharge from ER?
At a minimum, discharge instructions should include the diagnosis and treatment from the ER stay or hospitalization, a list of any prescriptions that need to be filled, details of any home health needs and providers that have been contacted, and what to do if the patient develop certain symptoms.
What are ER discharge papers?
What are ER discharge papers? A Discharge Paper is a sample form only for patients who are ready to leave the clinic or hospital. Through this form, there will be a smooth, easy process for both patients and staff. Before discharging patients from the hospital, certain information must be on file.
What should be included in a discharge letter?
Most discharge letters include a section that summarises the key information of the patient's hospital stay in patient-friendly language, including investigation results, diagnoses, management and follow up. This is often given to the patient at discharge or posted out to the patient's home.
What is the purpose of a discharge report?
The purpose of the discharge document is to summarize a patient's/client's progress toward goals, status at discharge, and future plans for self-management.
What information is on a hospital discharge summary?
Discharge summary This report is completed after the patient is discharged from the hospital. The report is a summary of the admission to the hospital, care provided, the diagnosis, procedures, medications, tests, immunizations, any problems and the plan for care after discharge from the hospital.
How do I write a letter of discharge?
As we discussed, I find it necessary to inform you that I will no longer be able to serve as your doctor as of (date at least 30 days from date of letter). The primary difficulty has been (indicate general reason, e.g., your failure to cooperate with the medical care plan, your behavior toward my staff, etc.).
What are 4 things that are required for a patient's successful discharge?
If the patient is being discharged to a rehab facility or nursing home, effective transition planning should do the following: ensure continuity of care. clarify the current state of the patientʼs health and capabilities. review medications. help you select the facility to which the person you care for is to be released.
What is included in discharge information?
Your discharge plan should include information about where you will be discharged to, the types of care you need, and who will provide that care. It should be written in simple language and include a complete list of your medications with dosages and usage information.
What information is on a discharge letter?
A hospital discharge letter is a brief medical summary of your hospital admission and the treatment you received whilst in hospital.It is usually written by one of the ward doctors.
What information is included in the Nurses discharge note?
The discharge instructions usually include a summary of the symptoms, diagnosis, diagnostic testing with the results, and the recommendations. Besides, the admitting provider describes the treatment plan and the patient's response to the prescribed plan. The patient's symptoms often improve or subside upon discharge.
What information should be included in a discharge summary quizlet?
Discharge summary is required for patient's stays greater than 48 hours.6 These components are: Reason for hospitalization. Significant findings. Procedures and treatment provided. Patient's discharge condition. Patient and family instructions (as appropriate). Attending physician's signature.
What information should be included in the discharge summary documentation?
To continue to paraphrase the APTA's description: All discharge summaries should include patient response to treatment at the time of discharge and any follow-up plan, including recommendations and instructions regarding the home program if there is one, equipment provided, and so on.
What information is important to provide the patient for discharge?
Provide Clear Discharge Instructions All instructions for care at home, including medications, diet, therapy, and follow-up appointments, must be explained in detail to all patients and then presented in written form to take home upon discharge. Exact dates and times of follow-up appointments need to be included.
What must be included in a discharge summary?
The discharge report must give a summary of everything the patient went through during the hospital admission period – physical findings, laboratory results, radiographic studies and so on. An AHRQ study points out that the Joint Commission mandates six components to be present in all U.S. hospital discharge summaries.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I manage my NHAMCS-173 directly from Gmail?
It's easy to use pdfFiller's Gmail add-on to make and edit your NHAMCS-173 and any other documents you get right in your email. You can also eSign them. Take a look at the Google Workspace Marketplace and get pdfFiller for Gmail. Get rid of the time-consuming steps and easily manage your documents and eSignatures with the help of an app.
How do I make edits in NHAMCS-173 without leaving Chrome?
Add pdfFiller Google Chrome Extension to your web browser to start editing NHAMCS-173 and other documents directly from a Google search page. The service allows you to make changes in your documents when viewing them in Chrome. Create fillable documents and edit existing PDFs from any internet-connected device with pdfFiller.
How can I edit NHAMCS-173 on a smartphone?
You can easily do so with pdfFiller's apps for iOS and Android devices, which can be found at the Apple Store and the Google Play Store, respectively. You can use them to fill out PDFs. We have a website where you can get the app, but you can also get it there. When you install the app, log in, and start editing NHAMCS-173, you can start right away.
What is NHAMCS-173?
NHAMCS-173 is a data collection tool used by healthcare facilities to gather information on outpatient services provided in the United States.
Who is required to file NHAMCS-173?
Health care providers and facilities that provide outpatient services and are selected to participate in the NHAMCS survey are required to file NHAMCS-173.
How to fill out NHAMCS-173?
To fill out NHAMCS-173, respondents need to provide accurate data on outpatient visit details, including patient demographics, visit outcomes, and resource utilization according to the provided guidelines.
What is the purpose of NHAMCS-173?
The purpose of NHAMCS-173 is to collect and analyze data to inform health policy and improve the quality of outpatient care in the U.S.
What information must be reported on NHAMCS-173?
NHAMCS-173 requires reporting of information such as patient demographics, diagnosis codes, treatment procedures, and patient outcomes during outpatient visits.
Fill out your NHAMCS-173 online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
NHAMCS-173 is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.