Get the free authorization letter for philhealth
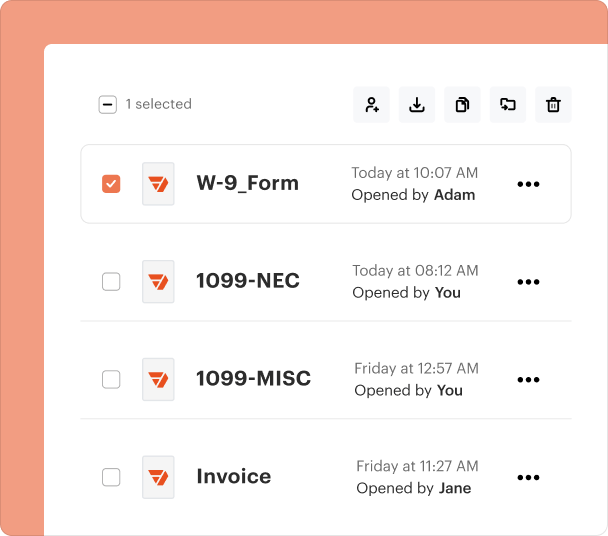
Fill out, sign, and share forms from a single PDF platform
Edit and sign in one place
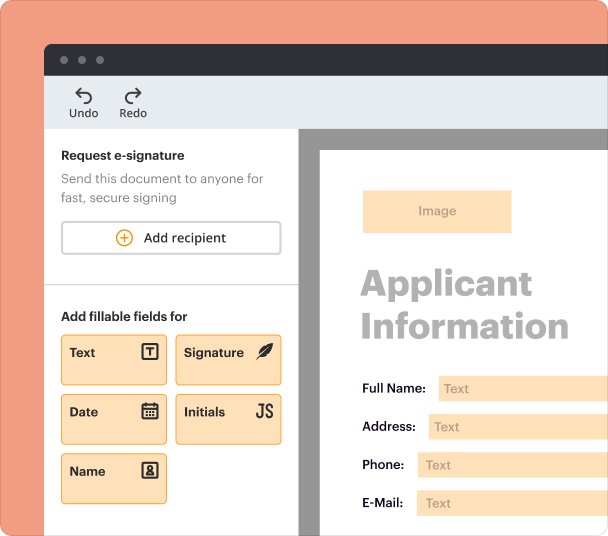
Create professional forms
Simplify data collection
Manage forms centrally
Why pdfFiller is the best tool for your documents and forms
End-to-end document management
Accessible from anywhere
Secure and compliant
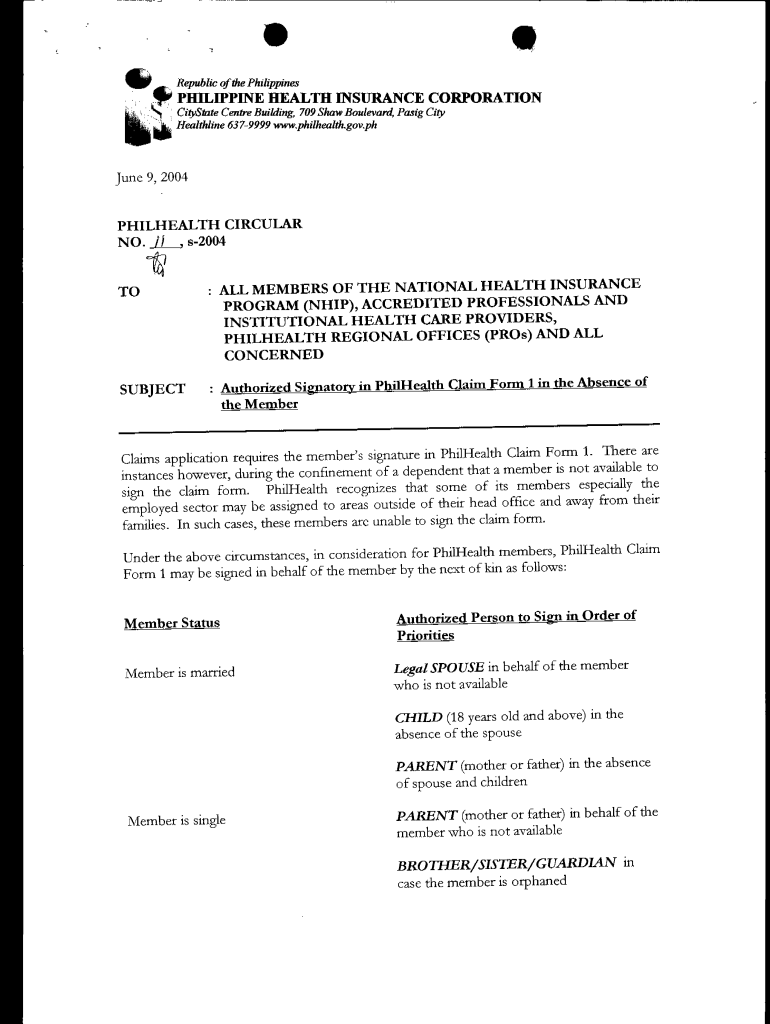
Authorization Letter for PhilHealth Form
What is an authorization letter?
An authorization letter serves as a formal document allowing one individual to act on behalf of another, particularly in healthcare settings like PhilHealth. This letter is crucial when a member is unable to submit claims themselves, thus facilitating the reimbursement process for medical expenses incurred.
-
It is a written permission that enables someone to act in the place of the PhilHealth member for claim submissions.
-
It plays a critical role in ensuring proper processing of claims, especially when the member is incapacitated.
When is an authorization letter needed?
An authorization letter is essential in instances where a PhilHealth member is unable to sign documents due to various reasons. Common situations include confinement in a hospital or being away from their usual residence.
-
Members may be hospitalized or traveling, making it impossible for them to handle their claims directly.
-
In cases where claims need to be filed for dependents or minors, an authorization letter is also required.
Who can sign on behalf of the member?
The authority to sign an authorization letter depends on the member's relationship and status. It's important for members to identify who can legally represent them in such transactions.
-
For married individuals, their spouse, children aged 18 and above, and parents can sign on their behalf.
-
Single members may have their parents, siblings, or guardians act as signatories, especially if they are without parents.
What documentation is required?
When initiating this process, specific documents must be submitted alongside the authorization letter to ensure efficient handling of claims.
-
This letter must detail the reasons behind its necessity.
-
Proof of identity and relationship with the member is crucial.
-
Including full name, unique address, and contact numbers for easy communication.
How to draft an authorization letter for PhilHealth?
Creating an effective authorization letter is integral for claim processing. The letter should adhere to a proper format and include all essential information.
-
The letter should begin with the date, followed by the member’s details, the nature of the authorization, and the signatory’s information.
-
Clarity is paramount; using clear headings and straightforward language will enhance understanding.
-
Consider using formal greetings when addressing PhilHealth representatives to maintain professionalism.
How to submit the authorization letter?
Once the authorization letter is prepared, the submission process must be followed accurately to avoid delays or complications in processing claims.
-
Ensure that all documents are complete and submit them in person or via designated channels outlined by PhilHealth.
-
Double-check the clarity and completeness of the submitted documents to avoid issues.
-
Understanding common pitfalls can help you navigate the submission process effectively.
What common issues arise with authorization letters?
Several challenges may surface when submitting authorization letters, often resulting in claim denials. Understanding potential issues can pave the way for prompt resolutions.
-
Incomplete information or incorrect signatory details can lead to quick rejections.
-
If a claim is denied, carefully review submission guidelines and rectify any identified issues.
-
Reach out to PhilHealth customer service or utilize online resources for help.
How can pdfFiller assist with document management?
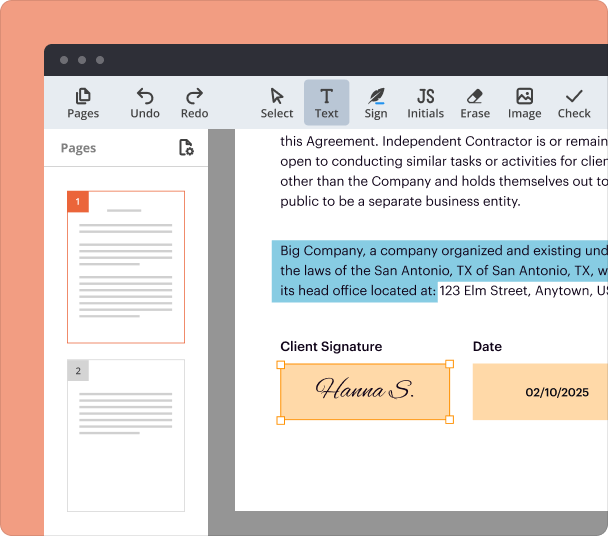
Using pdfFiller can significantly simplify the process of creating, editing, and signing your authorization letter, as well as other important documents.
-
Utilize pdfFiller’s intuitive platform for crafting precise authorization letters with ease.
-
Explore various tools for collaboration, signing, and secure storage of documents online.
-
A centralized platform enhances user experience while ensuring seamless document access from anywhere.
Frequently Asked Questions about philhealth authorization letter form
What is an authorization letter for PhilHealth?
An authorization letter for PhilHealth is a document that allows an individual to act on behalf of a member for claim submissions. This is especially important when the member is unable to handle their claims due to various circumstances.
How do I know if I need an authorization letter?
You typically need an authorization letter when you are unable to sign documents yourself, such as during hospitalization or travel. Additionally, dependents and minors seeking claims assistance also require this document.
Who can be my authorized signatory?
Authorized signatories include a spouse, children aged 18 or older, and parents for married members. Single members may use parents, siblings, or guardians if applicable.
What documents do I need to submit with the authorization letter?
You'll need to submit the authorization letter itself, a photocopy of the signatory's ID, proof of relationship with the member, and contact details for the signatory.
Can I use pdfFiller for my authorization letter?
Yes, pdfFiller offers an efficient platform for creating, editing, and managing your authorization letter and other documents. It streamlines the process and provides easy access to your documents online.
pdfFiller scores top ratings on review platforms