Get the free CT/CTA Prior Authorization Request Form
Show details
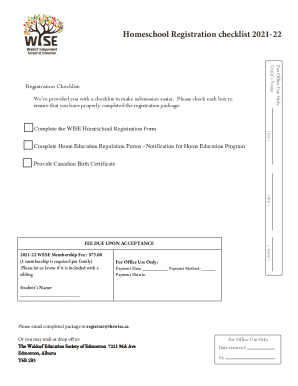
This form is used to request prior authorization for CT/CTA procedures, detailing patient information, symptoms, previous tests, and physician details.
We are not affiliated with any brand or entity on this form
Get, Create, Make and Sign ctcta prior authorization request

Edit your ctcta prior authorization request form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.

Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.

Share your form instantly
Email, fax, or share your ctcta prior authorization request form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit ctcta prior authorization request online
Use the instructions below to start using our professional PDF editor:
1
Set up an account. If you are a new user, click Start Free Trial and establish a profile.
2
Prepare a file. Use the Add New button to start a new project. Then, using your device, upload your file to the system by importing it from internal mail, the cloud, or adding its URL.
3
Edit ctcta prior authorization request. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
Dealing with documents is always simple with pdfFiller.
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
How to fill out ctcta prior authorization request

How to fill out CT/CTA Prior Authorization Request Form
01
Obtain the CT/CTA Prior Authorization Request Form from your healthcare provider or insurance company website.
02
Fill in patient information, including name, date of birth, and insurance details.
03
Specify the procedure or test being requested, including the reason for the request.
04
Include relevant medical history and any supporting documentation from the healthcare provider.
05
Sign and date the form, ensuring all sections are completed accurately.
06
Submit the form to the insurance company via mail, fax, or online portal as instructed.
Who needs CT/CTA Prior Authorization Request Form?
01
Patients who are scheduled for a CT or CTA scan.
02
Healthcare providers seeking approval for imaging tests to ensure coverage by insurance plans.
Fill
form
: Try Risk Free






People Also Ask about
How to do prior authorization for MRI?
Typically you call an imaging scheduling department and schedule the appointment, give them your insurance info, and they submit the authorization request to the insurance. You could also try calling your insurance company and asking them for preauthorization.
What are the requirements before a CT scan?
For four hours prior to your exam, please do not eat solid foods. You may drink fluids such as water, juice, or black decaffeinated coffee or tea. Some CT scan exams, particularly abdominal CT scans, may require that you drink water or an oral contrast so we may better visualize structures within the abdominal area.
Do you need informed consent for a CT scan?
If the patient undergoes the CT/MRI after having read the information sheet without asking for the radiologist, consent is implied. Private practices often play it safer by asking the patient to sign at the end of the information sheet while returning it back for legal documentation.
Is prior authorization needed for a CT scan?
Things like diagnostic images and complex care need prior authorization before you are treated. Prior authorization for MRIs and CT scans is standard. Your care provider will know to ask first, but don't be afraid to make sure. Each plan is different, so it's always good to ask.
Does a CT scan require prior authorization?
Examples of services or procedures for which prior authorization may be needed include: admission to a hospital or skilled nursing facility. planned surgery. certain imaging tests, like an MRI or a computed tomography (CT) scan.
What happens if you don't get prior authorization?
Prior authorization is not a guarantee that a claim will be approved, but failure to obtain prior authorization for a service that requires it will generally result in a claim denial. This is true even if the health plan would otherwise have covered the service.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What is CT/CTA Prior Authorization Request Form?
The CT/CTA Prior Authorization Request Form is a document required by healthcare providers to obtain approval from insurance companies before providing certain medical services or procedures.
Who is required to file CT/CTA Prior Authorization Request Form?
Healthcare providers and medical practitioners are required to file the CT/CTA Prior Authorization Request Form when they seek approval for specific diagnostic tests, treatments, or procedures that require prior authorization from the insurance company.
How to fill out CT/CTA Prior Authorization Request Form?
To fill out the CT/CTA Prior Authorization Request Form, the healthcare provider must provide patient information, details about the requested service or procedure, medical necessity justification, and any relevant clinical information or documentation required by the insurance company.
What is the purpose of CT/CTA Prior Authorization Request Form?
The purpose of the CT/CTA Prior Authorization Request Form is to ensure that the requested medical services or procedures are medically necessary and covered by the patient's insurance plan, thus preventing unnecessary costs for both the provider and the patient.
What information must be reported on CT/CTA Prior Authorization Request Form?
The information that must be reported on the CT/CTA Prior Authorization Request Form includes patient identification details, insurance information, provider information, specific procedure codes, diagnosis codes, and any supporting clinical documentation that establishes the medical necessity for the requested service.
Fill out your ctcta prior authorization request online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.

Ctcta Prior Authorization Request is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.