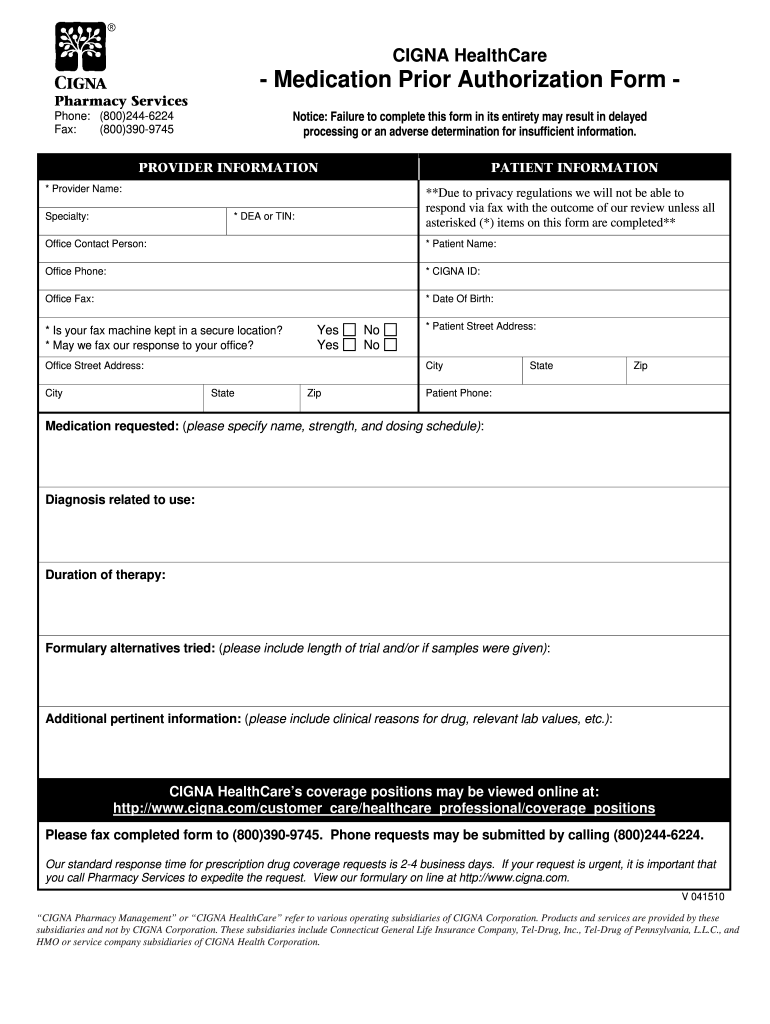
Cigna Medication Prior Authorization form 2010 free printable template
Show details
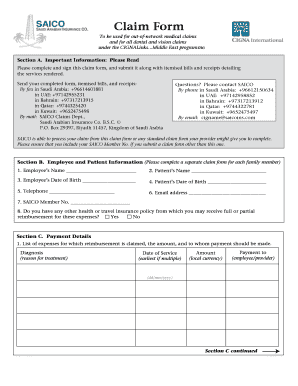
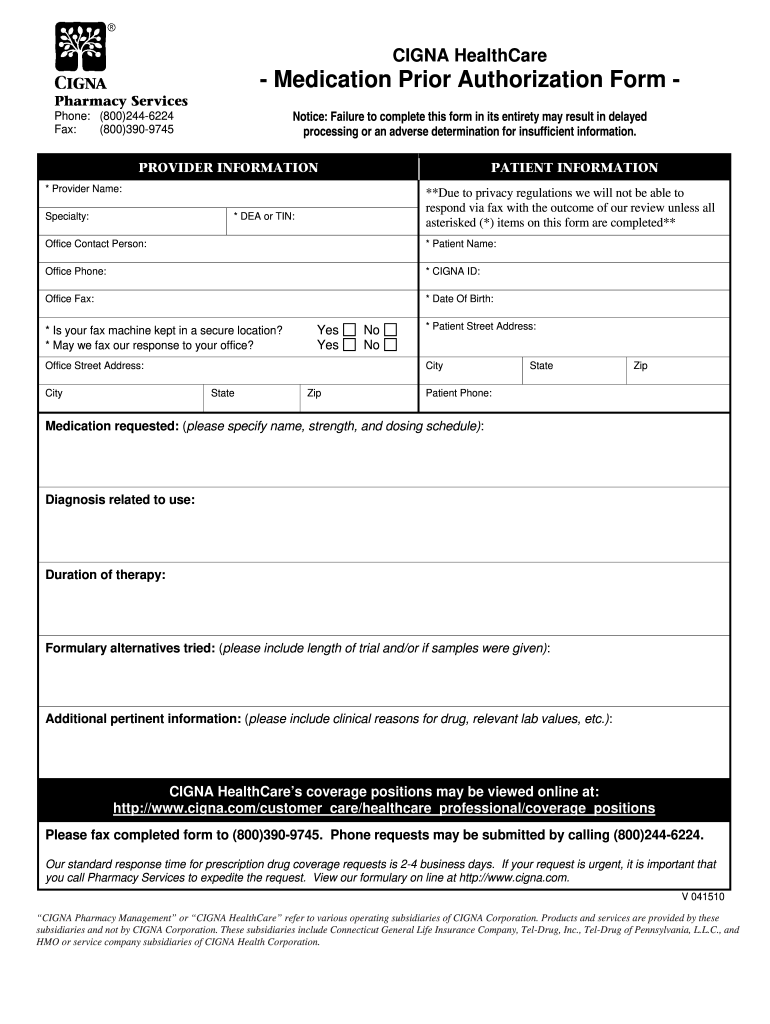
CIGNA HealthCare - Medication Prior Authorization Form Pharmacy Services Notice Failure to complete this form in its entirety may result in delayed processing or an adverse determination for insufficient information. Phone 800 244-6224 Fax 800 390-9745 PROVIDER INFORMATION PATIENT INFORMATION Provider Name Specialty Due to privacy regulations we will not be able to respond via fax with the outcome of our review unless all asterisked items on this form are completed DEA or TIN Office Contact...
pdfFiller is not affiliated with any government organization
Get, Create, Make and Sign Cigna Medication Prior Authorization form
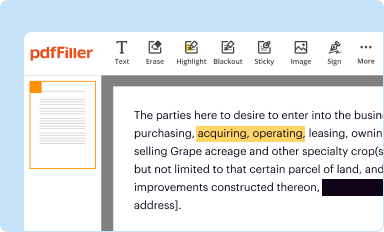
Edit your Cigna Medication Prior Authorization form form online
Type text, complete fillable fields, insert images, highlight or blackout data for discretion, add comments, and more.
Add your legally-binding signature
Draw or type your signature, upload a signature image, or capture it with your digital camera.
Share your form instantly
Email, fax, or share your Cigna Medication Prior Authorization form form via URL. You can also download, print, or export forms to your preferred cloud storage service.
How to edit Cigna Medication Prior Authorization form online
To use the professional PDF editor, follow these steps:
1
Check your account. If you don't have a profile yet, click Start Free Trial and sign up for one.
2
Upload a file. Select Add New on your Dashboard and upload a file from your device or import it from the cloud, online, or internal mail. Then click Edit.
3
Edit Cigna Medication Prior Authorization form. Rearrange and rotate pages, add new and changed texts, add new objects, and use other useful tools. When you're done, click Done. You can use the Documents tab to merge, split, lock, or unlock your files.
4
Save your file. Choose it from the list of records. Then, shift the pointer to the right toolbar and select one of the several exporting methods: save it in multiple formats, download it as a PDF, email it, or save it to the cloud.
pdfFiller makes dealing with documents a breeze. Create an account to find out!
Uncompromising security for your PDF editing and eSignature needs
Your private information is safe with pdfFiller. We employ end-to-end encryption, secure cloud storage, and advanced access control to protect your documents and maintain regulatory compliance.
Cigna Medication Prior Authorization form Form Versions
Version
Form Popularity
Fillable & printabley
How to fill out Cigna Medication Prior Authorization form
How to fill out Cigna Medication Prior Authorization form
01
Obtain the Cigna Medication Prior Authorization form from the Cigna website or your healthcare provider.
02
Fill in the patient's personal information, including name, date of birth, and insurance ID number.
03
Provide details about the medication requested, including the name, dosage, and frequency.
04
Include the healthcare provider's information, such as name, contact number, and specialty.
05
Document the medical diagnosis and relevant history that necessitates the prescribed medication.
06
Sign and date the form, confirming the information is correct and complete.
07
Submit the completed form to Cigna via their designated submission methods (fax, online, or mail).
08
Follow up with Cigna to ensure that the prior authorization is processed in a timely manner.
Who needs Cigna Medication Prior Authorization form?
01
Patients who require medication that is not covered under their health plan without prior authorization.
02
Healthcare providers who need to prescribe specific medications that require prior approval from Cigna.
03
Individuals seeking coverage for specialty pharmaceuticals or treatments that are subject to Cigna's prior authorization policy.
Fill
form
: Try Risk Free






People Also Ask about
What does preauthorized mean?
A decision by your health insurer or plan that a health care service, treatment plan, prescription drug or durable medical equipment is medically necessary. Sometimes called prior authorization, prior approval or precertification.
What is a preauthorized charge?
What is a pre-authorization? A pre-authorization is essentially a temporary hold placed by a merchant on a customer's credit card, and reserves funds for a future payment transaction. This hold typically lasts about five days, though this depends on your MCC (merchant classification code).
What is the point of pre-authorization?
The prior authorization process gives your health insurance company a chance to review how necessary a medical treatment or medication may be in treating your condition. For example, some brand-name medications are very costly.
What is a debit card preauthorization?
Pre-authorization makes sure the credit/debit card you provided has enough balance to cover future payments.
Does Cigna give refunds?
Any cancellation of membership in the Program will not affect any Services or discounts received by a canceling Member before the effective date of the cancellation. IF A MEMBER CANCELS WITHIN THIRTY (30) DAYS OF THE EFFECTIVE DATE, THE MEMBER WILL RECEIVE A FULL REFUND OF THE INITIAL MEMBERSHIP FEES. Membership Term.
What does it mean to Preauthorize a credit card?
Pre-authorizations reduce damages from fraud because if you choose to pre-authorize instead of transacting, and the customer happened to be using a fraudulent card, that customer can't issue a chargeback for that transaction because the funds were never actually used.
What does preauth mean on a bank statement?
A pre-authorization (also “pre-auth” or “authorization hold”) is a temporary hold on a customer's credit card that typically lasts around 5 days, or until the post-authorization (or “settlement”) comes through.
Can a pre-authorization be declined?
If a guest does not have enough funds to complete the actual transaction, the payment will be declined at close-out. If a guest has insufficient funds for the pre-authorization itself, then the transaction should be declined outright.
Can a debit card be pre-authorized?
If you're pre-purchasing before the planned release date, the credit/debit cards are pre-authorized when you initially order.
What does Preauthorised mean?
What is pre-authorisation? A pre-authorised transaction is where you take a deferred payment, rather than an immediate full payment, when a customer buys a product or service from you.
What is a pre-authorization hold on a credit card?
A pre-authorization hold simply confirms that funds are available on your credit or debit card. As soon as we can confirm that funds are available, we release the hold, returning it to your bank.
How long does it take to get approved for Cigna?
Typically, within 5-10 business days of receiving the prior authorization request, your insurance company will either: Approve your request. Deny your request.
How do debit card authorizations work?
Authorization holds work by connecting with the customer's bank or credit card provider to determine if there are enough funds to cover a charge. The funds are then placed on hold, which means the funds are no longer available to be used for other purchases.
How long do pre authorizations take?
How Does Prior Authorization Work? Most in-network providers submit a prior authorization request on your behalf. Still, it's always a good idea to check with your provider or a Personal Health Guide to ensure a particular procedure or service is approved. Prior authorization typically takes 7–14 business days.
How long does a pre-authorization stay on a debit card?
This is known as a pre-authorization hold. The merchant determines the amount of the hold. Typically the hold stays on your account until the funds are transferred to the merchant from your financial institution, often 3-4 days.
How does pre-authorization work on a credit card?
A credit card pre-auth is when a merchant reserves a transaction amount temporarily on a credit card, but only debits the amount after a few hours or days. This way, merchants can guarantee the availability of a payment amount for a specific transaction before it is finally confirmed.
What is a preauthorization charge on debit card?
A pre-authorization (also “pre-auth” or “authorization hold”) is a temporary hold on a customer's credit card that typically lasts around 5 days, or until the post-authorization (or “settlement”) comes through.
How do I complete a pre-authorisation?
In a virtual terminal Many virtual terminals have the option to choose preauthorisation as the “transaction type”. Once you've selected that, just fill in the required amount, card and customer details and click to complete the authorisation hold.
How long does it take to hear back from Cigna?
In most cases, it can take anywhere from one to three weeks to know if you've moved on to the interview stage after submitting your application. There are multiple factors that determine how long it takes for us to get back to you on next steps.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I fill out the Cigna Medication Prior Authorization form form on my smartphone?
Use the pdfFiller mobile app to fill out and sign Cigna Medication Prior Authorization form. Visit our website (https://edit-pdf-ios-android.pdffiller.com/) to learn more about our mobile applications, their features, and how to get started.
How can I fill out Cigna Medication Prior Authorization form on an iOS device?
Download and install the pdfFiller iOS app. Then, launch the app and log in or create an account to have access to all of the editing tools of the solution. Upload your Cigna Medication Prior Authorization form from your device or cloud storage to open it, or input the document URL. After filling out all of the essential areas in the document and eSigning it (if necessary), you may save it or share it with others.
How do I fill out Cigna Medication Prior Authorization form on an Android device?
Use the pdfFiller app for Android to finish your Cigna Medication Prior Authorization form. The application lets you do all the things you need to do with documents, like add, edit, and remove text, sign, annotate, and more. There is nothing else you need except your smartphone and an internet connection to do this.
What is Cigna Medication Prior Authorization form?
The Cigna Medication Prior Authorization form is a document used to request approval for certain medications before they can be covered by Cigna's insurance plan.
Who is required to file Cigna Medication Prior Authorization form?
Healthcare providers or prescribers are typically required to file the Cigna Medication Prior Authorization form on behalf of their patients.
How to fill out Cigna Medication Prior Authorization form?
To fill out the Cigna Medication Prior Authorization form, providers must include patient information, medication details, the reason for the request, and any relevant clinical information supporting the necessity of the medication.
What is the purpose of Cigna Medication Prior Authorization form?
The purpose of the Cigna Medication Prior Authorization form is to ensure that certain medications are medically necessary and appropriate for the patient before they are prescribed, in order to control costs and optimize patient care.
What information must be reported on Cigna Medication Prior Authorization form?
The information that must be reported includes the patient's name, date of birth, insurance details, medication name, dosage, the reason for the authorization request, relevant medical history, and clinical justification for the medication.
Fill out your Cigna Medication Prior Authorization form online with pdfFiller!
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.
Cigna Medication Prior Authorization Form is not the form you're looking for?Search for another form here.
Relevant keywords
Related Forms
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.