Understanding invasive group A streptococcus form: A comprehensive guide
Overview of invasive group A streptococcus (iGAS)
Invasive Group A Streptococcus (iGAS) refers to a severe form of the bacterium Streptococcus pyogenes that can cause life-threatening infections. This pathogen is typically known for its role in mild illnesses, such as strep throat or impetigo; however, when it invades deeper body tissues, it can lead to critical conditions requiring immediate medical attention. Understanding iGAS is vital for prevention and timely treatment, as early intervention can save lives.
iGAS infections are particularly concerning due to the rapid progression of symptoms and complications, posing a significant public health risk. High-risk populations include older adults, individuals with compromised immune systems, and those with chronic health conditions, making awareness and education crucial in combating the spread of these infections.
Understanding the pathogenesis of iGAS
The pathogenesis of invasive group A streptococcus involves several mechanisms that allow the bacteria to bypass the immune defenses. Once introduced into the body through breaks in the skin or mucous membranes, the bacteria can rapidly multiply and produce toxins that destroy surrounding tissue, promoting further invasion. This mechanism underscores the clinical severity associated with iGAS infections.
Common strains associated with these invasive infections include M1 and M3 types, which are particularly virulent. These strains produce virulence factors that enhance their ability to adhere to host cells and evade immune responses. Understanding these mechanisms helps in the development of targeted treatments and preventive strategies.
Symptoms of invasive group A streptococcus infection
Recognizing the symptoms of an invasive group A streptococcus infection early can drastically improve outcomes. Initial signs often include a sudden fever and chills, indicative of an infection. Skin lesions or rashes may also develop, often in the form of unusual or severe redness and swelling around a wound or a sore throat.
As the infection progresses, patients may experience severe pain in the affected area, which can be out of proportion to the physical findings. Other systemic symptoms such as nausea, vomiting, or dizziness may also appear. Special attention should be given to children, who may exhibit atypical symptoms such as irritability or lethargy.
Common diseases caused by invasive group A streptococcus
Invasive group A streptococcus can lead to several severe infections, including necrotizing fasciitis (often referred to as flesh-eating disease), streptococcal toxic shock syndrome (STSS), and pneumonia, among others. Each of these conditions presents with distinct clinical features but shares a common etiology with the iGAS bacteria.
Understanding the differences between mild and invasive forms is essential for effective treatment. While mild infections may resolve with basic antibiotic therapies, invasive forms require aggressive treatment strategies including potential surgical intervention.
Risk factors for invasive group A streptococcus
Several factors can increase the risk of contracting invasive group A streptococcus infections. High-risk groups often include very young children and older adults, as their immune systems may be less capable of fighting off infections. Individuals with pre-existing health conditions such as diabetes, heart disease, or those undergoing chemotherapy also exhibit increased susceptibility.
Additionally, recent invasive procedures or surgeries can provide an entry point for the bacteria. Seasonal influences also play a role; for instance, outbreaks of iGAS infections tend to be more frequent in colder months when respiratory infections are common.
Diagnosis of invasive group A streptococcus
Diagnosing iGAS often involves a combination of clinical evaluation and laboratory tests. Blood tests, including cultures and rapid antigen tests, are critical for confirming the presence of group A streptococcus in the bloodstream. Imaging studies, such as CT scans, may also be utilized to assess complications like abscess formation.
Early diagnosis is crucial, as prompt treatment can significantly lower the risk of severe complications or death. Therefore, healthcare providers must maintain a high index of suspicion when faced with symptoms indicative of invasive infections.
Treatment of invasive group A streptococcus
The treatment for invasive group A streptococcus typically involves high-dose intravenous antibiotics, with penicillin often being the preferred choice due to its effectiveness against this strain. Empirical therapy may initially include broad-spectrum antibiotics until the specific strain is identified.
Supportive care in a hospital setting is necessary, particularly for patients with severe symptoms requiring intensive monitoring. In cases of necrotizing fasciitis or other severe infections, surgical intervention may be required to remove dead tissue and prevent further spread of the infection.
Prevention strategies for invasive group A streptococcus
Prevention of iGAS primarily revolves around maintaining good personal hygiene practices. Regular handwashing, particularly after contact with sick individuals or healthcare settings, can significantly reduce the risk of transmission. Additionally, managing sore throats and skin infections promptly can mitigate the risk of progression to an invasive form.
It is essential to seek medical attention for non-invasive infections, as early treatment can prevent the progression to severe disease. Public awareness campaigns can also play a critical role in preventing outbreaks.
Health professional guidance and education
Post-infection care and monitoring are essential components of clinical management following an invasive group A streptococcus infection. Patients should be educated about the signs of recurrence and when to seek medical help. Access to educational resources such as pamphlets and digital materials can support patients and their families in understanding the condition.
Healthcare providers should also encourage ongoing training to recognize iGAS symptoms quickly and accurately, contributing to improved outcomes and reduced mortality rates. Engaging families in education can foster a collaborative approach to health management.
Interactive tools and resources
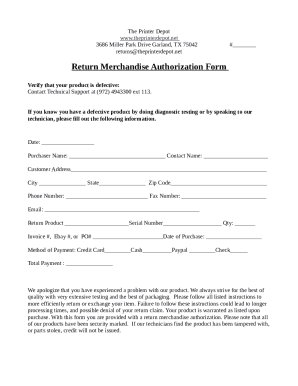
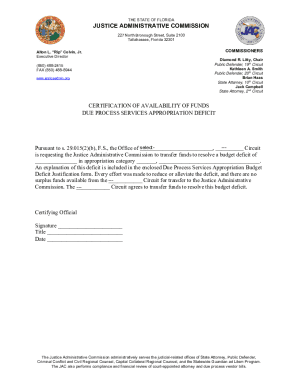
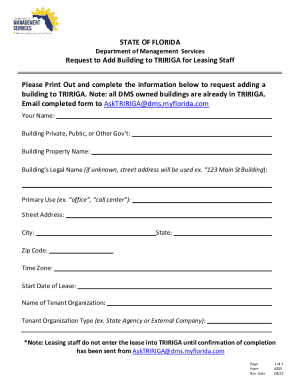
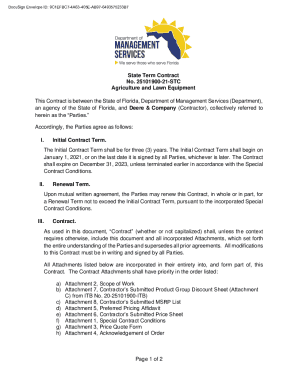
Utilizing interactive tools and resources can help manage health information related to invasive group A streptococcus infections. On pdfFiller, users can access various templates designed for tracking symptoms, medical history, and treatment plans. These tools enable individuals to document their health journeys effectively.
Filling out health forms accurately can streamline communication with healthcare providers. Templates available on pdfFiller promote thorough documentation, ensuring that critical details are not overlooked during medical consultations.
Community engagement and resources
Community engagement plays a vital role in raising awareness about invasive group A streptococcus. Schools and healthcare providers can collaborate to implement awareness campaigns, educating parents and caregivers about recognizing symptoms and understanding the risks associated with iGAS.
Resources for schools to manage outbreaks effectively, such as guidelines for reporting infections and educational materials for students and staff, are essential components of prevention and control strategies. Empowering communities with knowledge fosters a proactive approach to health and safety.
Frequently asked questions (FAQs)
Despite increasing awareness, misconceptions about iGAS persist. Common questions arise regarding the transmission, treatment efficacy, and preventative measures. For instance, people often wonder if iGAS infections can be contracted through casual contact, when in reality, they are typically spread through direct contact with infected wounds or respiratory droplets.
Schools play a crucial role in responding to cases of iGAS, with timely reporting and intervention strategies being essential to curb transmission. If symptoms of iGAS appear, individuals should seek medical attention promptly, emphasizing the importance of early diagnosis and treatment.
Stories and case studies
Real-life examples of invasive group A streptococcus infections illustrate the significant impact this condition can have on individuals and families. Sharing testimonials from health professionals and affected individuals can provide insights into the varied presentations of iGAS and underscore the importance of prompt intervention.
Case studies can highlight lessons learned and improvements made in treatment protocols, showcasing how community responses have evolved over time. These narratives can foster a deeper understanding of the disease's complexities and the need for continued vigilance.
Exploring further
Exploring connections between invasive group A streptococcus and other related conditions can enhance understanding of its complications and treatment. Emerging research continues to reveal novel insights into how iGAS interacts with the host’s immune system and the potential long-term effects of infections.
By keeping abreast of findings within the field, healthcare professionals can adapt their practices based on the latest evidence, ultimately improving patient outcomes. Encouraging ongoing research and discussions about iGAS will empower medical communities in their fight against this formidable pathogen.