Get the free () - Prior Authorization/Notification
Get, Create, Make and Sign prior authorizationnotification



Editing prior authorizationnotification online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorizationnotification

How to fill out prior authorizationnotification
Who needs prior authorizationnotification?
Prior Authorization Notification Form - How-to Guide
Overview of prior authorization notification forms
Prior authorization is a crucial component of the healthcare landscape, serving as a mechanism through which insurance providers confirm the medical necessity of treatments or medications before approving coverage. This ensures that patients receive appropriate care while simultaneously controlling costs for insurers. As a cornerstone of this process, the prior authorization notification form represents the bridge between healthcare providers, patients, and insurers.
Key stakeholders in this process include healthcare providers, who initiate requests; patients, who may require specific treatments; and insurers, who review and make decisions on authorization. Accurate documentation throughout this process is paramount, as any inconsistencies or errors could delay treatment for patients or lead to coverage denials.
Understanding the prior authorization process
For providers and patients alike, prior authorization signifies a necessary step to receiving medical care, especially for high-cost treatments or medications. This process can be particularly daunting for patients, who may face delays while waiting for approval, thereby hindering timely access to necessary treatments. Common reasons for requiring prior authorization include expensive procedures, specialty medications, and treatments deemed non-standard by the insurer.
Timeline expectations for approval can vary widely, with some requests being processed within a few days, while others might take weeks. Patients should be prepared for varying response times and communicate regularly with their healthcare providers to stay informed about their authorization requests.
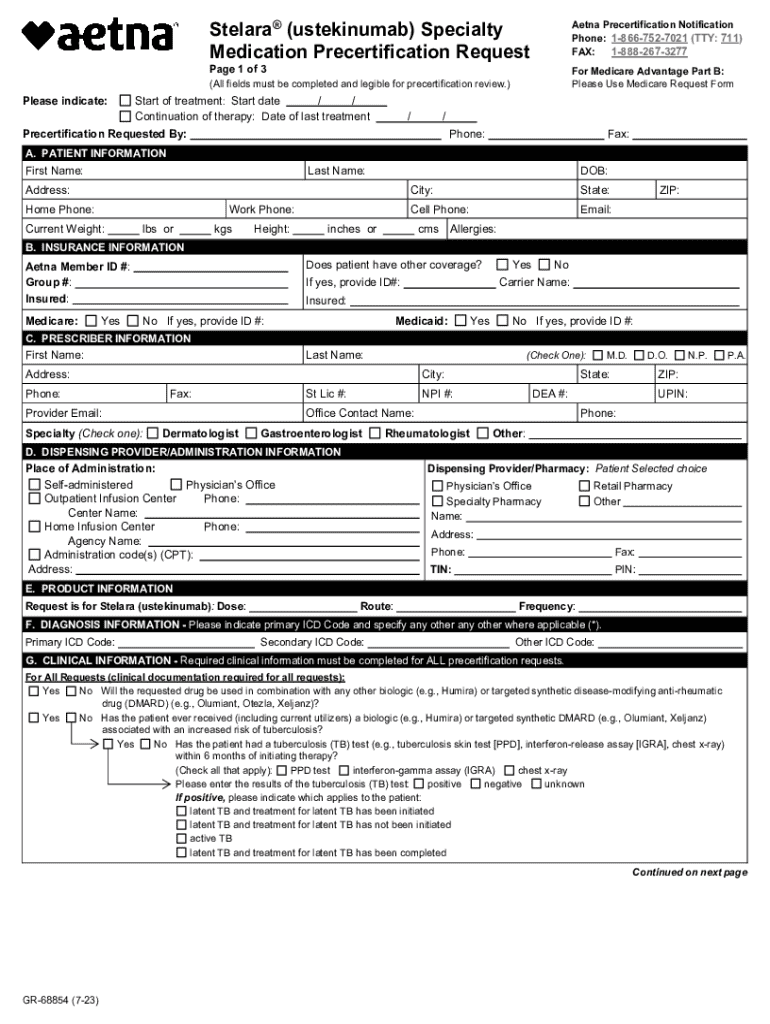
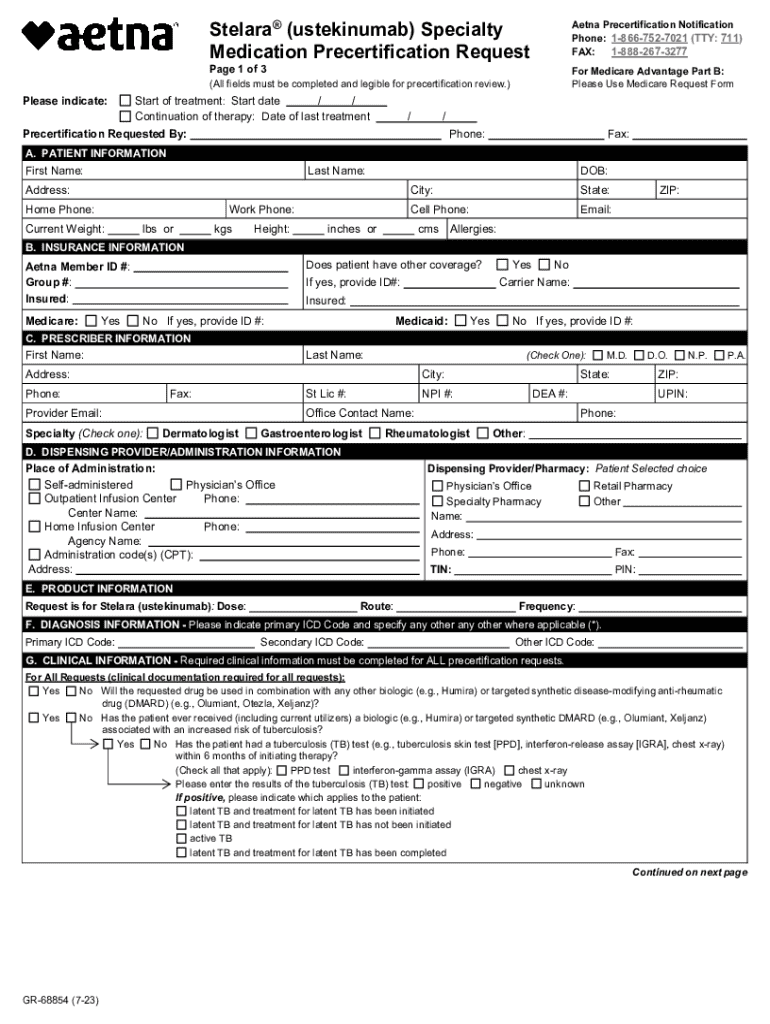
Navigating the prior authorization notification form
Structure of the form
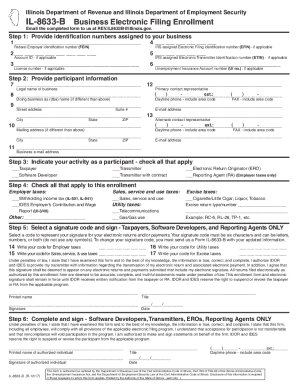
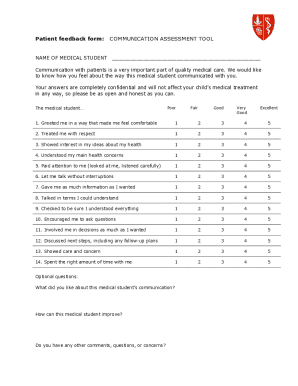
The prior authorization notification form comprises essential sections that facilitate clear communication between the provider and the insurance company. Key components typically include:
Sections explained
Each section plays a critical role in the prior authorization process. In the 'Patient Information' section, it is essential to include not just the basic demographics but also the patient's insurance policy details to avoid any processing delays. When detailing 'Procedure or Medication', clarity is paramount; specify the exact name, dosage, and reason it is warranted based on the patient’s medical history.
The 'Supporting Documents' section is equally vital: without adequate evidence of medical necessity, approvals can be delayed. Attach any relevant lab results, imaging reports, and treatment notes that can substantiate the request. Ensuring that these sections are thoroughly completed sets a strong foundation for a successful prior authorization.
Step-by-step instructions for completing the form
Gathering necessary information
Before starting on the form, gather the necessary information to ensure a smooth submission process. Compile all patient data, including personal details and insurance information. It is also essential to collect relevant previous medical records and supporting documents. This helps provide a clear picture of the patient's medical history and rationale for the treatment being requested.
Filling out the form
When it comes to filling out the form, accuracy is key. Begin by entering the patient’s information, then carefully describe the treatment or medication requested, ensuring to highlight any recent tests or recommendations from specialists. It’s recommended to double-check each field to minimize errors, as missing information can lead to delays in processing.
Reviewing your submission
Before submitting the prior authorization notification form, review your submission thoroughly. Check that all required fields are filled out completely and that the necessary supporting documents are attached. Common mistakes to avoid include typos in patient names or insurance details, as well as omitting required documentation. Completing this review can significantly improve the likelihood of swift approval.
Submitting the prior authorization notification form
Submission methods
Once the prior authorization notification form is complete, it's time to submit it to the insurance provider. There are generally two primary submission methods: electronic submission and fax. Electronic submissions can streamline the process, allowing for quicker delivery and the potential for real-time tracking of the submission's status. Conversely, faxing remains a common method, particularly where electronic systems are not robust, although it lacks the immediacy of digital methods.
Following up on your submission
After submission, it’s vital to track the status of the prior authorization request. Best practices include following up with the insurer to ensure the request is being reviewed within expected timeframes. Understanding the typical timelines and response expectations will empower providers and patients alike to navigate follow-up communications more effectively.
Enhancing collaboration and communication
Effective communication between providers and insurers is essential for successful prior authorization. Clear lines of communication can reduce misunderstandings and streamline the authorization process. Utilizing collaborative tools, such as shared platforms or digital e-signatures, can further enhance this communication, facilitating quicker approvals and transparency.
Encouraging feedback allows for continuous process improvement, enabling healthcare providers and insurance companies to refine workflows and reduce turnaround times for prior authorizations. Establishing a culture of open communication fosters stronger partnerships between these key stakeholders.
Innovations in prior authorization processing
Technological advancements are transforming the prior authorization landscape. Software solutions and AI tools now offer sophisticated means to automate and streamline the prior authorization notification form submission process, dramatically reducing the time spent on paperwork. Tools like pdfFiller exemplify this innovation, allowing users to edit PDFs directly within the application, collaborate in real-time with teams, and utilize e-signature capabilities to accelerate the process.
The integration of such technologies not only enhances efficiency but also aids in achieving better outcomes for patients by reducing delays associated with authorization processes.
Common challenges and solutions
The submission of prior authorization requests can be fraught with challenges. Frequent obstacles include insufficient documentation, overlooked requirements for specific treatments, and long waiting periods for approvals. To overcome these challenges, providers can establish a systematic approach to document collection and verification before submission.
Employing a checklist that outlines all necessary documentation and steps can significantly streamline the process and enhance efficiency. Additionally, keeping abreast of changes in insurer policies and coverage criteria allows providers to adapt quickly and avoid unnecessary delays.
Best practices for efficient prior authorization management
Establishing a streamlined workflow is paramount for efficient prior authorization management. Healthcare providers should develop an internal protocol that clarifies the roles and responsibilities of staff members involved in the process. This includes setting timelines for information gathering and regular follow-ups on submissions. Staying informed about changes in insurance coverage criteria, treatment guidelines, and policy updates can help healthcare teams remain proactive in managing prior authorizations.
Regular training sessions for staff on best practices for documentation and compliance can lead to improved accuracy and efficiency, ultimately benefiting patient care and satisfaction.
Real-life case scenarios
Examining real-life case scenarios can provide valuable insights into the effective management of prior authorization requests. For instance, a healthcare provider faced with delayed treatments due to incomplete submissions may adopt a team-based approach for reviewing requests before submission, ensuring that multiple eyes verify the completeness of documentation.
Lessons learned from challenges faced, such as navigating particularly complex medications that require extensive documentation, highlight the importance of establishing clear communication channels with insurance representatives. Successfully addressing these challenges can lead to improved processes and better patient outcomes.
Conclusion on effective prior authorization processes
In conclusion, efficient management of prior authorization notification forms is critical for ensuring timely access to necessary healthcare treatments. Organizations that prioritize precision in documentation and leverage tools like pdfFiller to manage their processes effectively will likely see significant benefits in terms of both patient care and operational efficiency.
By committing to best practices, facilitating clear communication, and staying updated on policy changes, healthcare providers can navigate the complexities of prior authorization with confidence.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I modify my prior authorizationnotification in Gmail?
How can I get prior authorizationnotification?
Can I create an eSignature for the prior authorizationnotification in Gmail?
What is prior authorization notification?
Who is required to file prior authorization notification?
How to fill out prior authorization notification?
What is the purpose of prior authorization notification?
What information must be reported on prior authorization notification?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.