Get the free Request for Prior Authorization - cloudfront.net
Get, Create, Make and Sign request for prior authorization



How to edit request for prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out request for prior authorization

How to fill out request for prior authorization
Who needs request for prior authorization?
How to effectively request a prior authorization form
Understanding prior authorization
Prior authorization is a critical component of the healthcare system, functioning as a gatekeeper to ensure that specific medical services or medications are necessary and justifiable. Its primary purpose is to secure insurance coverage for patients, helping avoid unexpected out-of-pocket expenses later on. This process is especially important in situations where costly treatments are involved, as it allows insurers to review the medical necessity based on standardized criteria.
Reasons for requesting prior authorization
There are several common scenarios when prior authorization is required. Medications that are deemed high-cost or experimental typically necessitate this approval, as do specialized procedures that may not be universally accepted across all insurance plans. For physicians, obtaining prior authorization can help them provide better patient care by ensuring that the treatments they recommend are covered by insurance, which boosts patient adherence to prescribed therapies.
The necessity of the prior authorization form
Using the prior authorization form is essential when dealing with insurance policies that require it for certain healthcare services. Typically, this happens when specific treatments are identified as needing further justification before proceeding. There is a clear distinction between outpatient and inpatient requests, where outpatient services might require quicker turnaround times, whereas inpatient procedures may involve a more detailed review process.
Potential obstacles in the process
A common frustration for many patients and healthcare providers is the risk of request denials. Requests can be denied for a multitude of reasons, often tied to insufficient documentation or lack of clarity regarding medical necessity. The importance of accurate information cannot be overstated; ensuring that all details are precisely outlined on the request is vital for successful authorization.
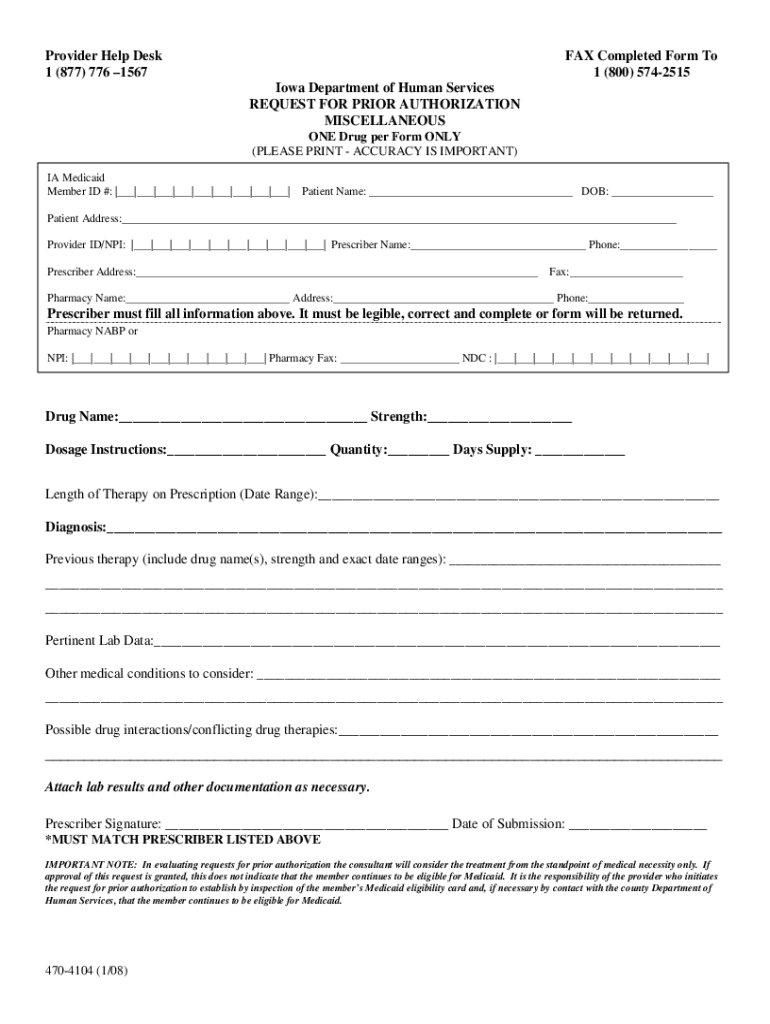
Getting started with the request for prior authorization form
To initiate a prior authorization request, it’s crucial to locate the correct form. Typically, this form can be found on the healthcare provider's website or the insurance company’s portal. pdfFiller simplifies this process greatly. Users can easily locate and access the necessary forms online, allowing for a more efficient authorization process.
Prerequisites before filling out the form
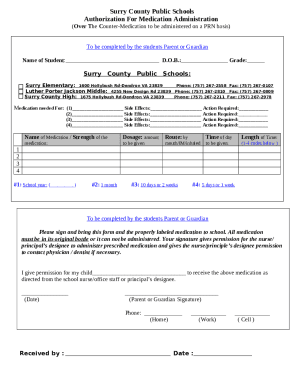
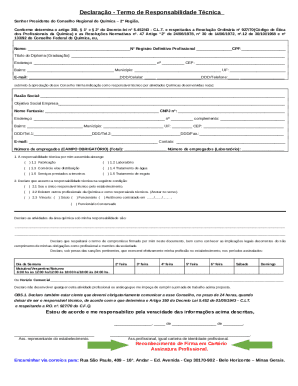
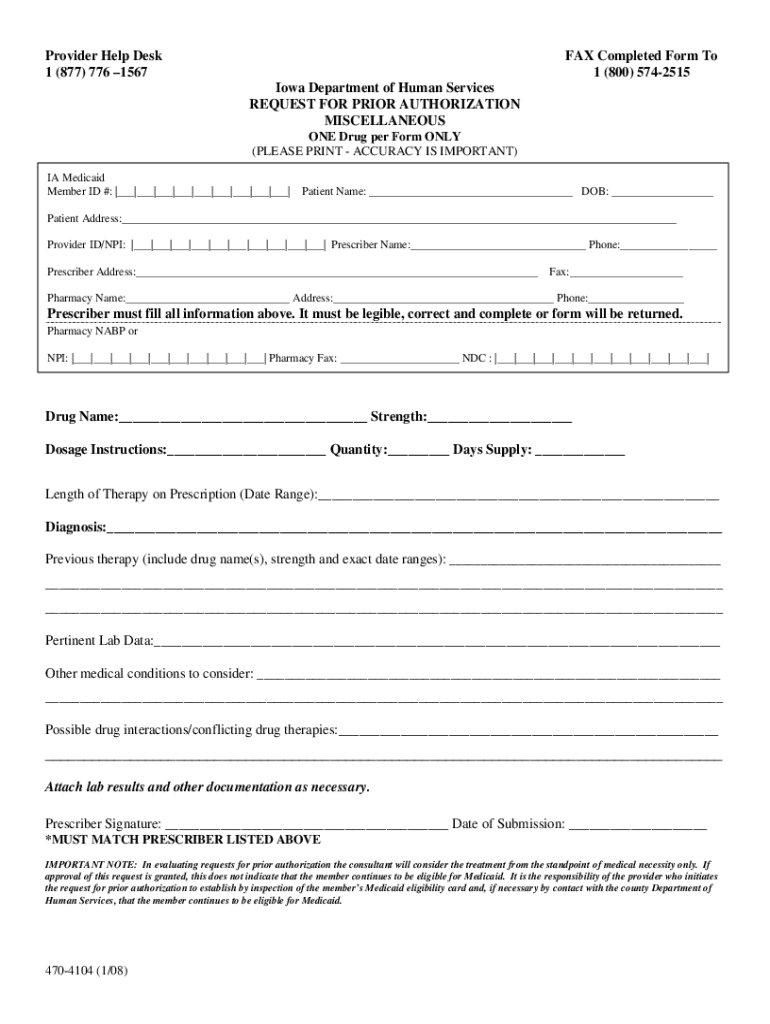
Before beginning the completion of the request for prior authorization form, gather essential patient information. This typically includes the patient’s name, contact details, insurance data, and relevant medical history. Ensuring that all information is complete and accurate is of utmost importance, as inaccuracies can lead to audit flags or denials.
Detailed steps to complete the prior authorization form
Completing the prior authorization form requires attention to detail across several key steps. Starting with personal and patient information, make sure to include all necessary details to clearly identify the patient and their insurance coverage. This initial step is foundational; errors here can lead to complications later in the process.
Submitting the form
After completing the form, deciding on the method of submission is crucial. Options generally include e-filing or physical submission by mail. Utilizing pdfFiller not only facilitates the completion of the form but also allows for seamless online submission directly to the insurance provider.
Expected timeframe for response
Anticipating the timeframe for a response to the prior authorization request is essential. Most insurance providers typically respond within a few business days for standard requests, while more complex cases might extend the timeframe. It's vital to understand these differences to manage patient expectations and coordinate care effectively.
Following up on your request
After submission, tracking the status of your prior authorization request is key. Many insurance companies provide a contact number or an online portal to check on your application’s status. Utilizing tools available through pdfFiller, users can keep track of submissions and follow up with necessary inquiries to the insurance company.
Next steps if denied
If a request for prior authorization is denied, there are specific steps to take. First, it’s essential to review the reasons for denial carefully. Depending on the outcome, appealing the decision is often the next course of action. It's beneficial to gather additional documentation and provide a detailed explanation of medical necessity in the appeal.
Tips for successful prior authorization requests
Filling out prior authorization forms accurately is a skill that can greatly enhance the chance of approval. Best practices include being clear and concise in detailing the medical necessity, as well as ensuring all forms are fully completed. Documenting the rationale for treatment succinctly can help insurance representatives quickly understand the need.
Common mistakes to avoid
Some errors frequently encountered in prior authorization requests can lead to unnecessary delays or outright denial. These include submitting forms with incomplete patient information or failing to thoroughly explain medical necessity. In addition, skipping the review process before submission might result in overlooked errors that could hinder approval.
Utilizing pdfFiller for an enhanced submission experience
pdfFiller stands out as a transformative tool for managing the prior authorization process. With its user-friendly features designed for editing, signing, and sharing documents, users can efficiently navigate the complexities associated with form submissions. The platform's cloud-based system ensures that documents are accessible from any device at any time.
Collaborating with teams through pdfFiller
Effective collaboration among healthcare teams is vital for successful prior authorization requests. pdfFiller’s platform simplifies this process, allowing for seamless sharing and editing of documents among providers, administrative staff, and patients. Utilizing cloud access fosters enhanced communication and documentation management.
Additional considerations
Different insurance policies can significantly impact the prior authorization process. Each insurer may interpret prior authorization requirements differently, so being aware of specific policy provisions is crucial for healthcare providers. Additionally, staying updated on policy changes will help streamline the approval process in future requests.
Resources for further assistance
For those seeking additional resources or clarification about prior authorization processes, professional associations and helplines can be highly beneficial. Collaborating with healthcare providers to gather the necessary information or to address unclear areas can also significantly aid in the request process.
The final review of the prior authorization process
Following the steps and protocols outlined above ensures a smooth and efficient prior authorization process. Proper documentation and submission not only optimize approval chances but greatly enhance the overall experience for both patients and healthcare providers. Leveraging technology, particularly through platforms like pdfFiller, can lead to increased accuracy and efficiency.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I create an electronic signature for signing my request for prior authorization in Gmail?
Can I edit request for prior authorization on an iOS device?
How do I complete request for prior authorization on an Android device?
What is request for prior authorization?
Who is required to file request for prior authorization?
How to fill out request for prior authorization?
What is the purpose of request for prior authorization?
What information must be reported on request for prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.