Resources on Prior and Form
Understanding prior authorization and forms
Prior authorization is a crucial step in the healthcare system, designed to ensure that certain medical services or medications are necessary before financial coverage is granted by insurance providers. This process involves a detailed review of the patient's medical history and the justification for the requested service or medication. For healthcare providers, understanding the nuances of prior authorization is essential to streamline patient care and avoid delays in treatment.
The importance of prior authorization cannot be understated. It serves as a gatekeeping mechanism to control healthcare costs and ensure that patients receive clinically appropriate services. This means that patients are less likely to undergo unnecessary procedures, which can further complicate their health and increase overall expenses.
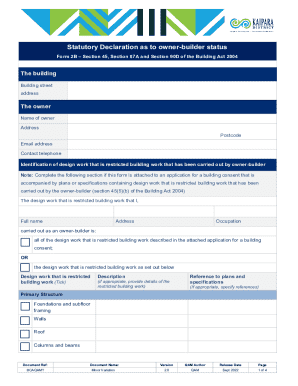
Forms play a pivotal role in the prior authorization process. Proper completion of these forms ensures that all necessary information is provided to support the request. Insurers often have specific forms for different types of requests, necessitating familiarity with these documents for timely processing.
Types of prior authorization requests
Prior authorization requests can typically be categorized into two main types: medication and non-medication requests. Each category comes with its own nuances regarding required information and handling protocols.
Medication prior authorization requests often require detailed information about the patient's medical history and the rationale for prescribing a specific drug. Non-medication requests, on the other hand, could involve procedures, specialist referrals, or tests that require similar justification. Appropriate forms must be used for each type.
These requests necessitate documentation of medical necessity, previous treatments, and relevant lab results.
Involves services like surgeries, imaging, or specialized therapies requiring specific justification.
These are time-sensitive cases where treatment cannot wait for standard approval timelines.
Specific forms tailored to the different types of prior authorization requests must be utilized.
The prior authorization process
Submitting a prior authorization request involves several critical steps. Understanding each step ensures that, as a healthcare provider or administrative team, you can facilitate quicker approvals and enhanced patient care.
Collect all relevant patient data, including medical history, treatment plans, and any previous therapy responses.
Ensure accuracy in completing the required form, providing detailed clinical justification to support the request.
Choose the submission method preferred by the insurance provider, ensuring all submitted documents are clear and legible.
Expediting the prior authorization process requires understanding key payer requirements. Each insurance company may have differing stipulations on the data necessary for a successful approval. Ensuring compliance with these guidelines significantly paves the way for a seamless submission process.
Furthermore, familiarizing oneself with regulatory considerations, such as HIPAA compliance, can prevent potential legal issues that may arise during the authorization process.
Interactive tools and resources
To simplify the complexities involved with prior authorizations, numerous interactive tools and resources can be utilized. These tools not only help with submission but also enhance collaboration and tracking.
Many insurers provide dedicated online platforms for users to submit forms, track request status, and maintain communication.
Insurance companies often offer template forms tailored to specific requests, enhancing efficiency in documentation.
pdfFiller allows users to edit documents in real-time and facilitates easy collaboration through cloud-based solutions.
Navigating the challenges of prior authorizations
Prior authorizations, while necessary, pose several challenges, including delays in approvals and complications in submitting forms. Understanding common obstacles can equip providers to tackle them proactively.
Frequent administrative errors, lack of information, and extended review times from insurers.
Implementing thorough checks before submission and maintaining open lines of communication with payers.
In the case of a denial, knowing the correct procedures for appeals is vital to overturn the decision.
When dealing with denied requests, specific steps should be followed. First, gather all related documentation that outlines the case, then prepare a persuasive appeal that clearly states the reasoning for reconsideration. Presenting this information succinctly and with supporting evidence dramatically increases the likelihood of a successful appeal.
As healthcare practices become more complex, adapting to the evolving world of prior authorization is pivotal, allowing for smoother operations and ultimately better patient care.
Best practices for providers and teams
To ensure effective management of prior authorization processes, healthcare providers should implement best practices that streamline workflows and enhance communication.
Establish clear communication channels to minimize misunderstandings and speed up resolutions.
Regular training sessions on prior authorization processes and new changes can keep teams knowledgeable and efficient.
Stay informed about new healthcare regulations that impact prior authorization to ensure compliance.
Creating structured workflows can help prioritize and manage incoming requests effectively.
By committing to these best practices, healthcare teams can ensure that they are equipped to handle the demands of prior authorization efficiently, thereby improving the overall patient experience.
Statistical insights and case studies
Understanding the impact of prior authorization through statistics and real-world examples can inform better practices. Research indicates that nearly 90% of healthcare providers encounter challenges when dealing with prior authorization, with over 30% reporting that these challenges negatively affect care delivery.
Studies show longer wait times lead to increased patient dissatisfaction and higher operational costs.
Examples from leading healthcare practices demonstrate how improved protocols and technology can streamline authorization.
Healthcare professionals share their experiences and tips for minimizing bottlenecks in prior authorization.
By examining these insights, healthcare organizations can assess their processes critically and identify areas for improvement, ultimately leading to enhanced operational efficiencies.
Comprehensive resource center
A well-curated resource center can be invaluable for individuals and teams navigating the complexities of prior authorization. This center provides access to essential documents and helpful guides.
Access a variety of forms required for submission, avoiding pitfalls of incomplete documentation.
A compilation of frequently asked questions provides quick answers to common inquiries.
Familiarize with common terminology to enhance communication and workflow in documentation.
Having these resources readily available leads to more efficient processes and less confusion among team members when working through prior authorizations.
Support and contact information
Effective support systems are critical for addressing issues that may arise during the prior authorization process. Organizations should ensure that they have accessible support avenues.
Dedicated support lines or chat services should be established for urgent queries.
Regular check-ins with support teams can foster relationships that enhance issue resolution.
Collaborating with pdfFiller can provide enhanced document management tools that streamline prior authorization forms.
Efficient solutions to technical challenges surrounding prior authorization can drastically reduce the burden on healthcare teams, enabling them to focus more on patient care.
Additional learning opportunities
Continued education is essential for evolving alongside the healthcare landscape. Various learning opportunities can enhance understanding of prior authorizations.
Regularly scheduled sessions cover new updates and best practices related to prior authorization.
Flexible online modules can help teams learn at their own pace while mastering critical knowledge.
Connecting with other professionals offers insights into how different organizations manage prior authorizations.
Through active participation in these learning opportunities, healthcare providers can remain informed and adept at navigating the complexities of prior authorizations.