Get the free Vanflyta (quizartinib) Prior Authorization Form
Get, Create, Make and Sign vanflyta quizartinib prior authorization



How to edit vanflyta quizartinib prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out vanflyta quizartinib prior authorization

How to fill out vanflyta quizartinib prior authorization
Who needs vanflyta quizartinib prior authorization?
Navigating the Vanflyta Quizartinib Prior Authorization Form
Understanding the Vanflyta Quizartinib prior authorization process
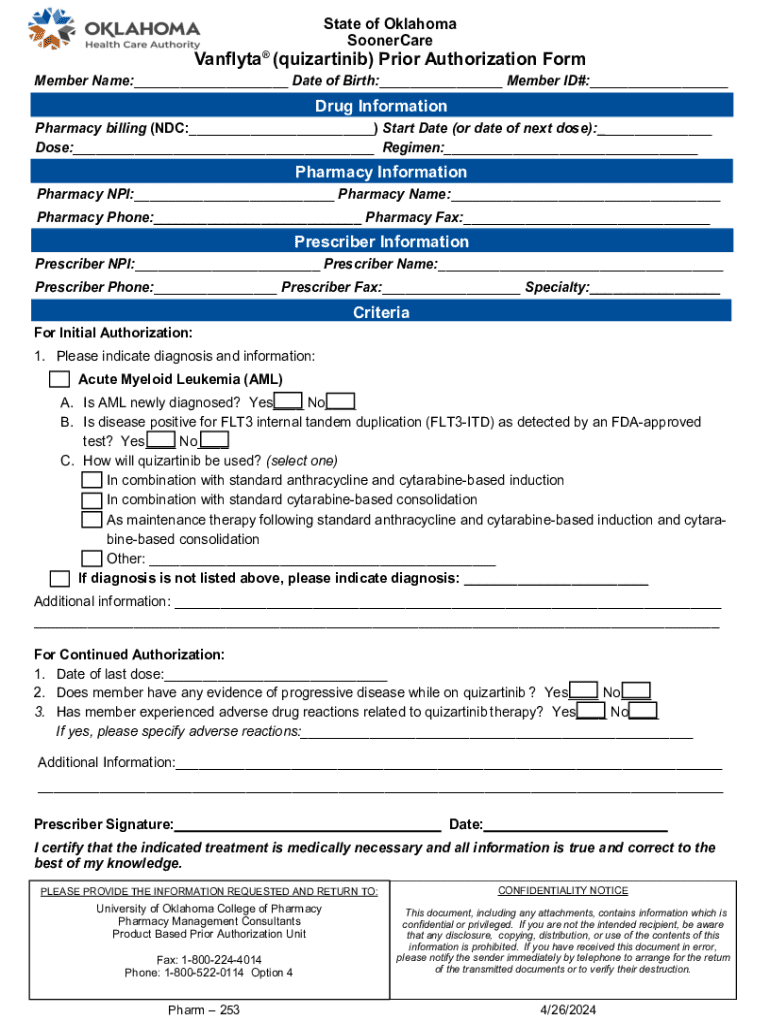
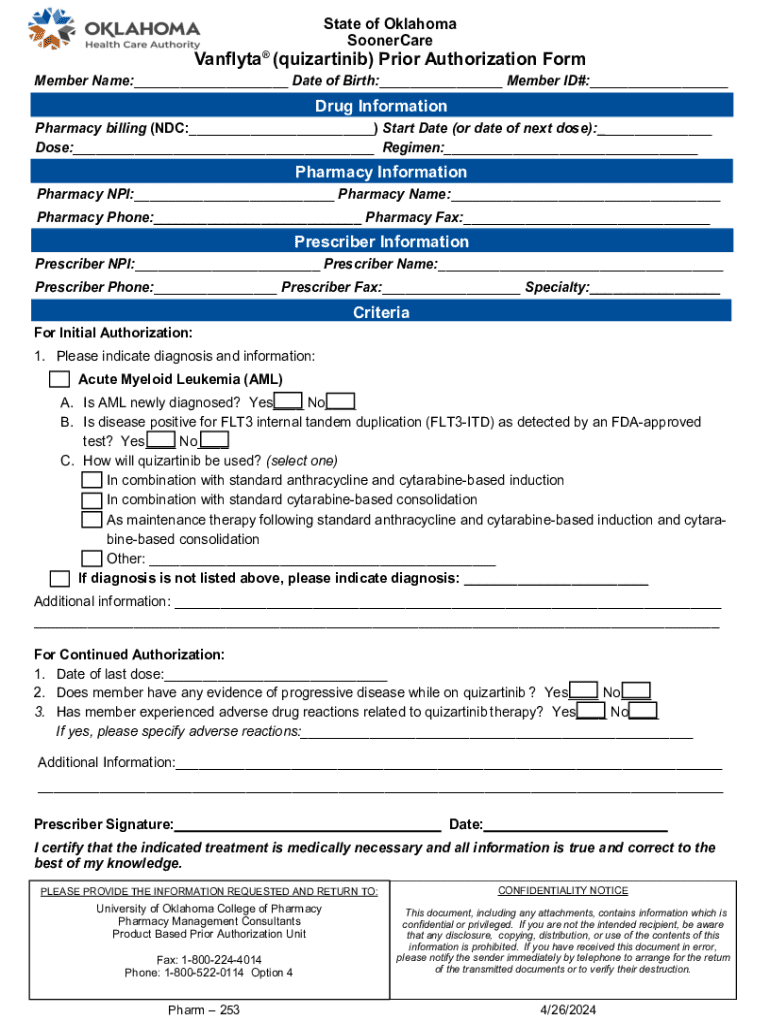
Prior authorization is an essential process in which healthcare providers must obtain approval from a patient's insurance company before certain medications can be prescribed. This process often applies to high-cost prescription drugs, such as Vanflyta (quizartinib), which is used in the treatment of specific types of leukemia. This article is designed to guide both individuals and teams through the detailed steps required to successfully complete the Vanflyta quizartinib prior authorization form.
Proper documentation plays a crucial role in this process. Accurate and comprehensive information on the authorization form can facilitate quicker approval and reduce the chances of denial. The Vanflyta quizartinib authorization form must include not only patient-specific data but also details that justify the medical necessity of the drug for the individual in question.
Preparing for the authorization submission
Before submitting the authorization request, it is essential to gather all required information. This includes patient identifiers such as their full name, date of birth, insurance policy number, and contact information. Additionally, a thorough understanding of the patient's diagnosis and medical history will be critical. This information should comprehensively detail the patient's previous treatments, response to those treatments, and the rationale for why quizartinib is being proposed.
Moreover, a detailed treatment plan specification should be prepared. This includes expectations for the length of therapy with quizartinib, any concurrent medications being prescribed, and relevant lab results that support the treatment plan. Understanding key terms such as 'prior authorization,' 'quizartinib,' and 'medical necessity' is also beneficial for effectively navigating the forms and potential discussions with insurance representatives.
Step-by-step guide to filling out the authorization form
To access the Vanflyta quizartinib authorization form, it can typically be obtained in multiple formats, including PDF or web-based formats. It's important to obtain the most current version of the form to avoid submission delays. As you delve into completing the form, each section should be treated with careful attention to detail.
The authorization form generally consists of several key sections, including Patient Information, Provider Information, Medical Information, and Justification for Therapy. Start by filling in the Patient Information section with accurate identifiers, followed by the Provider Information which includes the prescribing physician's details. The Medical Information section necessitates a detailed report on the patient's health condition and history, while the Justification for Therapy section should highlight why quizartinib is critical for treatment, citing any previous therapies the patient has undergone.
Additionally, it’s crucial to avoid common mistakes such as leaving sections incomplete or incorrectly inputting data. Errors can lead to delays in the authorization process or even outright denials, necessitating resubmission.
Editing and customizing the authorization form
Using tools like pdfFiller enhances the process of editing and customizing the authorization form. This platform provides features for altering fields, adding necessary notes, and more, allowing healthcare providers to tailor the document precisely to their needs. Users can edit text specific to their patient's situation, which is vital for a personalized approach to the form.
Moreover, pdfFiller offers eSigning capabilities, which enable quick approval once the form is finalized. This functionality reduces turnaround time for obtaining necessary signatures from providers or patients. Teams can also collaborate within the platform, where they can share the form, comment on sections, and make real-time edits, fostering a more efficient workflow.
Submitting the Vanflyta quizartinib authorization form
Once the authorization form is completed, the next step is to submit it to the appropriate insurance provider. Comprehensive submission instructions should accompany the form, guiding where to send it, whether via fax or online submission channels. Most insurance providers have specific fax numbers or dedicated portals for electronic submissions that ensure faster processing.
Follow-up is crucial after submission. Tracking authorization status is often possible through the provider's website or by calling customer service. Be prepared to respond promptly to any requests for additional information from the insurance company, as this can significantly impact the approval timeline.
Understanding coverage and reauthorization guidelines
Understanding the criteria for approval is essential when dealing with the Vanflyta quizartinib prior authorization form. Generally, medical necessity forms the cornerstone of approval, meaning that evidence supporting the need for quizartinib must be clearly articulated and documented. Evidence such as treatment history, lab results, and other relevant data should be emphasized in your authorization request.
Reauthorization is another critical aspect that healthcare professionals must manage. This process typically requires resubmitting information periodically to confirm that continued treatment is necessary. Providers should be aware of specific timelines and documentation needs for reauthorization to avoid interruptions in patient care. Common reasons for denial include insufficient information or a lack of documented medical necessity.
Managing your documentation with pdfFiller
Using pdfFiller for document management bolsters efficiency across the authorization process. With its cloud-based features, users can securely organize, store, and retrieve forms and records. This ensures that all documentation is accessible from any location, reducing the chances of paperwork getting lost, and enhancing the overall workflow.
Additionally, pdfFiller allows users to manage access and permission settings, making it easy to control who can view or edit specific documents. By integrating pdfFiller with tools used in healthcare settings, users can streamline their overall document workflow, reducing time spent on administrative tasks and concentrating more on patient care.
Frequently asked questions about the authorization process
When a prior authorization is denied, it can be frustrating for both healthcare providers and patients. Understanding what to do next is crucial. Many times, audit trails can be requested to gain insight into the reasons behind denials. Knowing how to expedite the authorization process can also prove beneficial. For example, submitting all required documentation on the first attempt can help facilitate quicker responses.
If additional information is needed following an initial denial, providing a comprehensive appeal letter outlining new evidence or additional support can help strengthen the case. For first-time applicants navigating this process, having a checklist of required documents and understanding submission guidelines can significantly ease the journey.
Additional resources for healthcare providers
Healthcare providers striving for a comprehensive understanding of quizartinib and its associated protocols can benefit from accessing updated guidelines and educational materials. This could include varieties of continuing education programs that discuss the specifications regarding prior authorization and specific pharmaceutical treatments, including quizartinib.
Connecting with other medical professionals for insights and advice related to the authorization process is also highly recommended. Additionally, resources like pdfFiller offer customer support and expert guidance in documenting effectively, allowing healthcare providers to stay informed on the best practices for filling out forms like the Vanflyta quizartinib prior authorization form.
Staying updated on policy changes
The landscape of drug coverage and authorization procedures is constantly evolving, requiring vigilance from healthcare professionals. Staying abreast of policy changes regarding drug approvals, such as those pertaining to quizartinib, is critical for ensuring that patient care remains uninterrupted. Regularly reviewing the authorization procedures set forth by insurance companies and pharmaceutical guidelines can significantly benefit healthcare providers.
Adopting a proactive approach to understanding these policies not only aids individual practitioners but can also support healthcare teams in advocating for their patients, ensuring they receive the medications necessary for their health and recovery.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I edit vanflyta quizartinib prior authorization from Google Drive?
Can I sign the vanflyta quizartinib prior authorization electronically in Chrome?
How can I edit vanflyta quizartinib prior authorization on a smartphone?
What is vanflyta quizartinib prior authorization?
Who is required to file vanflyta quizartinib prior authorization?
How to fill out vanflyta quizartinib prior authorization?
What is the purpose of vanflyta quizartinib prior authorization?
What information must be reported on vanflyta quizartinib prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.