Specialized and focused geriatric form: A how-to guide
Understanding the specialized geriatric form
A specialized geriatric form is essential for documenting the unique needs and challenges faced by older adults in a healthcare setting. These forms capture critical information about a patient’s medical history, cognitive function, and daily living abilities, providing a clear picture of their overall health status.
Accurate documentation through specialized forms is foundational in geriatric care. It facilitates appropriate care planning and fosters effective communication among healthcare providers, family members, and caregivers. A well-structured geriatric form ensures that vital details are not overlooked, ultimately leading to improved patient outcomes.
Definition: A specialized form tailored to the needs of elderly patients.
Purpose: To document essential healthcare information and treatment planning.
Importance: Accurate data collection leads to tailored healthcare interventions.
Types of geriatric forms
Different aspects of geriatric care necessitate various specialized forms. These forms include but are not limited to medical history forms, cognitive assessment forms, and functional ability assessment forms. Each type serves a specific purpose and is designed to gather relevant information that can inform individualized care strategies.
For example, medical history forms are vital to understanding chronic conditions, while cognitive assessment forms gauge mental acuity. Functional ability assessment forms evaluate an elderly patient’s capacity for daily activities, ensuring that caregivers can effectively support their needs.
Medical History Forms: Capture patients’ medical backgrounds and chronic conditions.
Cognitive Assessment Forms: Evaluate cognitive health and identify potential impairments.
Functional Ability Assessment Forms: Assess daily living capabilities and independence.
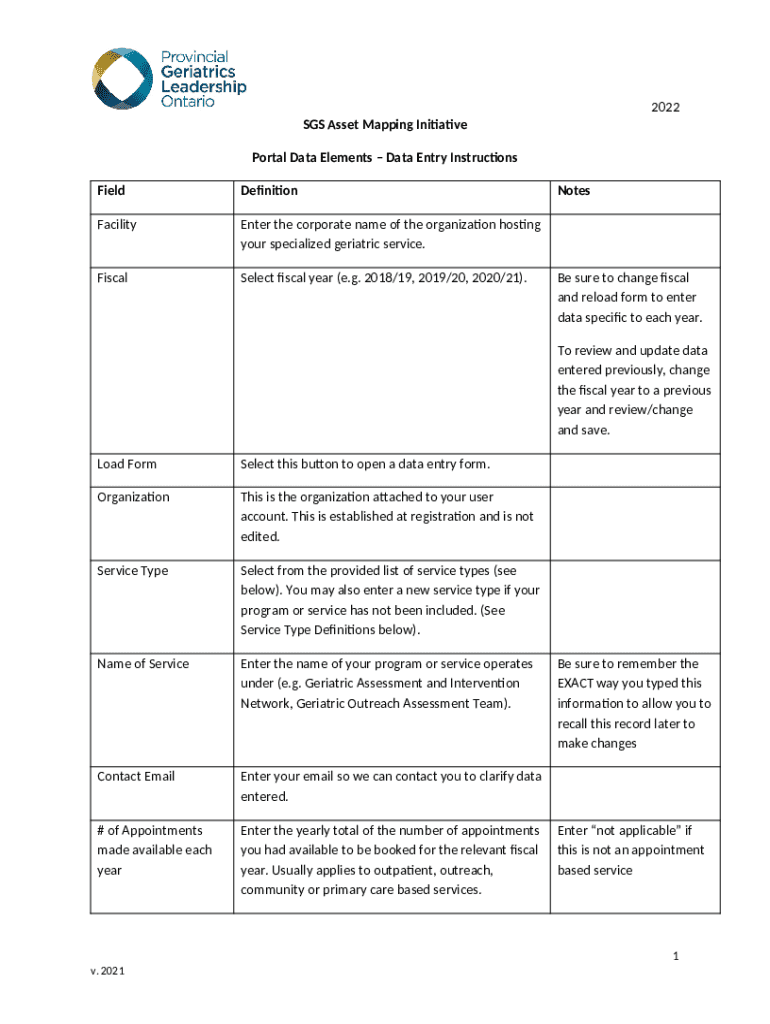
Step-by-step instructions for filling out geriatric forms
Filling out geriatric forms accurately is crucial, and breaking the task into manageable steps can simplify the process. Start by identifying the required sections on the form and ensuring that all necessary areas are addressed. It’s imperative to utilize available patient history to inform your entries, ensuring comprehensive documentation.
When documenting patient information, consistency is vital. Report symptoms precisely, and avoid vague terms to reduce the risk of miscommunication. Collaborative input from family members and healthcare teams can provide a fuller picture of the patient’s health, making it easier to create an effective care plan.
Identify Required Sections: Know which parts of the form must be filled out for accuracy.
Utilize Patient History: Refer to existing records to ensure thorough documentation.
Consistency in Reporting: Ensure that symptom descriptions are detailed and clear.
Collaborative Input: Engage families and healthcare teams for comprehensive input.
Editing and managing geriatric forms with pdfFiller
pdfFiller offers an intuitive interface for managing geriatric forms efficiently. Users can upload existing forms or utilize templates to maintain consistency across documentation. The platform ensures that the forms remain accessible from any location, simplifying collaborative efforts among healthcare teams.
Additionally, pdfFiller provides interactive tools for enhancing documentation. Users can add annotations, comments, and even refer to video tutorials to optimize their use of the platform. This functionality enhances the quality and accuracy of documentation, ultimately benefiting the patient.
Uploading Existing Forms: Seamlessly integrate current documentation into the platform.
Using Templates: Ensure consistency and ease of use across documentation.
Adding Annotations: Enhance forms with comments and notes for better clarity.
eSigning and securing geriatric documents
The use of eSignatures in healthcare documentation is paramount. It not only streamlines the signing process but also enhances the security of sensitive information. With pdfFiller, electronic signatures are integrated seamlessly, ensuring that all documents are signed quickly and remain compliant with healthcare regulations.
Users can customize the signing process, allowing for flexibility in how forms are shared and completed. Furthermore, pdfFiller includes features to ensure that all documents adhere to compliance and security standards that protect patient privacy.
Importance of eSignature: Increases efficiency in document turnaround and signing.
How to Electronically Sign: Simple steps to add eSignatures to your forms.
Ensuring Compliance: Features that help maintain the security of patient information.
Collaborating on geriatric forms
Collaboration is often necessary when managing geriatric forms, as multiple stakeholders may need to provide input. pdfFiller facilitates easy sharing of forms with both healthcare teams and family members. Users can work together in real-time, making updates and providing feedback to ensure that the documentation is accurate and comprehensive.
Moreover, pdfFiller includes tools for maintaining version control and audit trails. This feature is critical in healthcare settings, as it ensures that all changes are tracked and that stakeholders can easily refer back to previous versions when necessary.
Sharing Forms: Easy collaboration among healthcare teams and family members.
Real-Time Updates: Enhance accuracy through immediate feedback and input.
Version Control: Track changes and maintain clear documentation history.
Common challenges in managing geriatric documentation
Healthcare providers often face challenges when managing geriatric documentation, particularly with patients experiencing cognitive impairments. Strategies for caregivers to address these challenges include employing patience, simplifying explanations, and using relatable examples to overcome communication barriers.
Ensuring the accuracy of documentation is another key challenge. Inconsistent reporting can lead to miscommunication among care teams. Thus, protocols should be established to maintain thorough and accurate notes on patient information. Additionally, caregivers must remain vigilant about the sensitivity of information, especially regarding privacy laws.
Addressing Cognitive Impairment: Tips for effective communication with patients.
Ensuring Accuracy: Protocols to maintain consistency in reporting.
Handling Sensitivity: Awareness of privacy laws and regulations governing documentation.
Quality improvement in geriatric care documentation
Completed geriatric forms can serve as valuable tools for quality assurance and improvement. Healthcare providers can review these documents to establish benchmarks for geriatric care practices and identify areas for enhancement. By assessing performance based on completed forms, attention can be given to gaps in care and opportunities for professional development.
Continuous learning is vital for healthcare teams involved in geriatric care. Engaging in training programs and utilizing specialized resources can foster an environment of ongoing improvement, leading to better patient outcomes.
Using Completed Forms: Assessing performance against benchmarks and care standards.
Establishing Benchmarks: Setting key performance indicators for care practices.
Continuous Learning: Incentivizing ongoing education for care teams.
Specialized resources for geriatric forms
Various resources are available to support healthcare providers in efficiently managing geriatric forms. Checklists and quality improvement tools can help ensure that all aspects of the documentation process are addressed effectively, enhancing the quality of care delivered to elderly patients.
Educational materials and training programs specialized in geriatric care documentation can equip providers with the skills required to navigate challenges they may face. Additionally, joining support networks focused on geriatric care can provide valuable insights and shared experiences for professionals in this field.
Recommended Checklists: Tools to streamline the documentation process.
Accessing Educational Materials: Training resources for healthcare providers.
Joining Support Networks: Platforms for sharing insights and experiences.
Prioritizing patient-centered care in geriatric documentation
At the heart of effective geriatric care is a patient-centered approach, which is reflected in how forms are designed and utilized. Gathering patient feedback can significantly enhance the usability and relevance of geriatric forms. By tailoring forms to meet the individual needs of patients, providers can ensure that each document is relevant and beneficial.
Empathy and communication are essential components of patient-centered care. Practitioners should prioritize understanding patient concerns and incorporating their preferences into documentation practices. This approach not only enriches the patient experience but also fosters a stronger relationship between caregivers and elderly patients.
Role of Patient Feedback: Enhancing forms based on direct user input.
Tailoring Forms: Adapting documentation to meet individual patient needs.
Importance of Empathy: Building trust and understanding with elderly patients.
Frequently asked questions about geriatric forms
Law-related concerns often arise around geriatric documentation. Understanding the legal aspects regarding patient information is paramount for providers. It is crucial to know how to handle sensitive data ethically and legally, ensuring compliance with healthcare standards.
Common issues that practitioners may encounter when dealing with geriatric forms include completeness, accuracy, and formatting. By identifying potential obstacles early on, solutions can be implemented effectively. Providers can also seek out resources for additional support and information to better manage geriatric documentation.
Clarifications on Legal Aspects: Understanding compliance and confidentiality obligations.
Troubleshooting Common Issues: Strategies for overcoming documentation challenges.
Resources for Support: Where to find additional information and guidance.
Next steps in utilizing geriatric forms effectively
Implementing best practices in everyday clinical use of geriatric forms is crucial for effective documentation. Encouraging a culture of continuous improvement within healthcare teams can foster a commitment to high-quality patient documentation and care. Leveraging pdfFiller's features can streamline the documentation process, enhancing both efficiency and accuracy.
Overall, by following a structured approach, healthcare providers can navigate the complexities associated with geriatric care documentation. Continually adapting to new tools and processes will empower teams to deliver the highest standard of care to their elderly patients.
Implementing Best Practices: Ensure accuracy and thoroughness in documentation.
Encouraging Continuous Improvement: Foster an environment of collaboration and growth.
Leveraging pdfFiller: Utilize the platform for efficient geriatric form management.