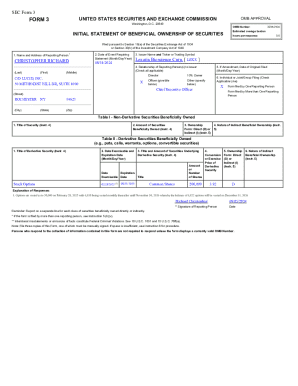
Get the free Prior Authorization (PA) Form for Insulins
Get, Create, Make and Sign prior authorization pa form



How to edit prior authorization pa form online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization pa form

How to fill out prior authorization pa form
Who needs prior authorization pa form?
Prior Authorization PA Form: A Comprehensive How-to Guide
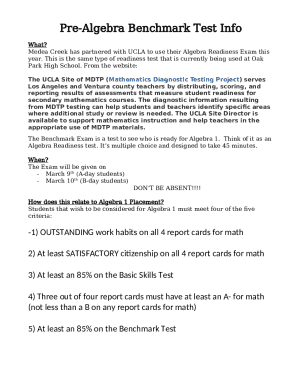
Understanding prior authorization
Prior authorization is a critical process in the healthcare system whereby insurance providers approve certain medical services or medications before they are delivered to the patient. This step ensures that the proposed treatments align with the patient's medical needs and the insurance company's policy guidelines.
The necessity of prior authorization stems from the need to control healthcare costs, prevent unnecessary procedures, and ensure the treatment's medical necessity. It's commonly required for high-cost medications, advanced imaging tests, and any specialized treatment plans.
Overview of the prior authorization PA form
The prior authorization PA form is a crucial document submitted to healthcare insurers to request approval for specific medical services or medications. This form outlines the patient's medical history, the requested treatment, and the justification for medical necessity.
Its importance cannot be overstated as it serves as a gatekeeper for access to necessary medical care. Insurance companies use the information provided in this form to evaluate whether the treatment is appropriate or exceeds standard medical guidelines.
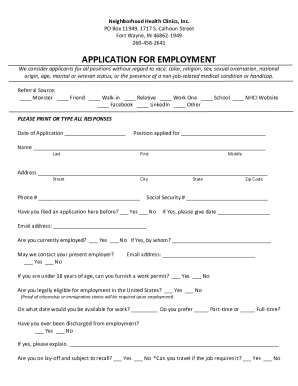
Steps to obtain a prior authorization PA form
Obtaining a prior authorization PA form begins with identifying your health insurance provider. Start by accessing their official website or contacting customer service for information regarding the necessary forms.
Upon identifying your insurance provider, follow these steps to locate the correct prior authorization PA form:
Detailed instructions for completing the prior authorization PA form
Completing the prior authorization PA form accurately is essential for a smooth approval process. Understanding the sections of the form will help ensure all necessary information is included.
Here’s a breakdown of what to include in each section:
Common mistakes include providing incomplete information, failing to include relevant medical documents, or neglecting to clarify treatment expectations. Taking careful time to double-check the information will minimize the chances of any errors.
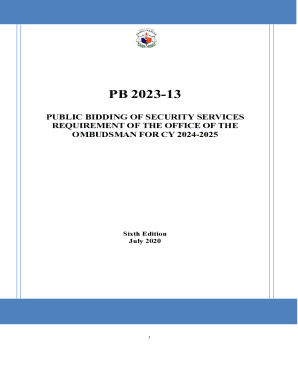
Editing and managing your prior authorization PA form
Once you have completed the prior authorization PA form, managing it effectively is key to retaining control over your healthcare documentation. pdfFiller simplifies document management and offers powerful editing tools.
Utilizing pdfFiller, you can easily edit your prior authorization form by following these steps:
Tips for successful submission of the prior authorization PA form
Submitting your prior authorization PA form requires attention to detail to ensure it successfully reaches the insurance provider. Here are some recommended submission methods and practices:
Collaborating with healthcare teams during prior authorization
Collaboration among healthcare teams can significantly aid in navigating the prior authorization process. Roles can vary, with healthcare providers, administrative staff, and even patients playing key parts.
Using innovative tools like pdfFiller enhances collaboration by enabling real-time editing and e-signing. This ensures that all parties have access to the most current versions of the documents, which facilitates a faster processing time.
Managing denials and appeals
Receiving a denial for your prior authorization request can be disappointing, but understanding the potential reasons can help mitigate future issues. Common denial reasons may range from incomplete forms to a lack of medical necessity.
If your prior authorization is denied, here are steps to take to file a successful appeal:
Conclusion: Streamlining your prior authorization process
In conclusion, mastering the prior authorization PA form is crucial for accessing necessary medical treatments. Leveraging efficient, access-from-anywhere solutions like pdfFiller not only weaves through the complexities of documentation but also enhances collaboration among healthcare teams.
Investing in a streamlined approach to managing your healthcare forms can greatly reduce stress and improve outcomes. With pdfFiller’s capabilities, users can confidently address prior authorization processes and focus more on what truly matters—their health.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make changes in prior authorization pa form?
Can I create an electronic signature for the prior authorization pa form in Chrome?
How can I edit prior authorization pa form on a smartphone?
What is prior authorization pa form?
Who is required to file prior authorization pa form?
How to fill out prior authorization pa form?
What is the purpose of prior authorization pa form?
What information must be reported on prior authorization pa form?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.