Get the free Medicaid Managed Care Reenrollment Member Request Form - eohhs ri
Get, Create, Make and Sign medicaid managed care reenrollment



How to edit medicaid managed care reenrollment online
Uncompromising security for your PDF editing and eSignature needs
How to fill out medicaid managed care reenrollment

How to fill out medicaid managed care reenrollment
Who needs medicaid managed care reenrollment?
Medicaid Managed Care Reenrollment Form - How-to Guide
Understanding Medicaid managed care reenrollment
Medicaid managed care is a system where Medicaid benefits are delivered through private health plans, focusing on comprehensive, coordinated care. Reenrollment in Medicaid managed care is essential as it ensures that beneficiaries maintain their coverage and receive essential health services without interruptions. Furthermore, recent key changes in Medicaid policies could affect your coverage options, making timely reenrollment critical for your ongoing healthcare needs.
Eligibility requirements for reenrollment
To qualify for Medicaid managed care reenrollment, applicants must generally meet specific eligibility criteria. This typically includes being a resident of the state where you are applying and demonstrating financial need based on income guidelines set by Medicaid. Special considerations may also apply to families and individuals with disabilities to ensure their distinct needs are supported adequately.
Preparing for the reenrollment process
Before starting the reenrollment process, gathering essential documents is vital. This includes proof of income, identification documents, and your previous Medicaid or CHIP number. Being organized ensures a smoother application process. Additionally, understanding deadlines and renewal timelines can prevent unnecessary lapses in coverage.
Step-by-step guide to completing the Medicaid managed care reenrollment form
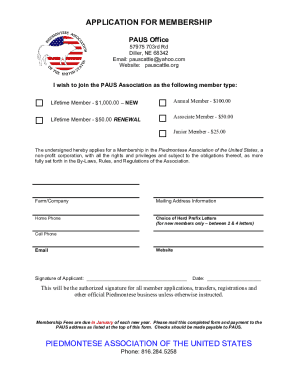
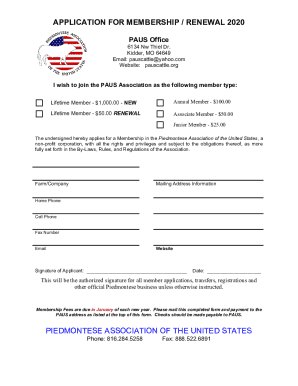
Accessing the form
To access the Medicaid managed care reenrollment form, visit your state’s Medicaid website or locate it through pdfFiller. The form is typically available in various formats, including PDFs for printing and online submission options, allowing for greater flexibility in how you complete your application.
Filling out the form: detailed instructions
Completing the form correctly is crucial. Start by filling out personal information accurately. Follow with household information, ensuring all members are included. Income details should reflect your current financial situation, and finally, answer any additional questions and certifications honestly, as they can impact your eligibility.
Common mistakes to avoid
Many applicants make avoidable errors that can delay the application process or even lead to denial. Ensure all information provided is accurate and complete. Missing supporting documents can trigger requests for additional information, wasting time and effort. Lastly, never leave sections blank, as this can be interpreted as incomplete information leading to potential denial.
Review and submit your application
Once the form is completed, take a moment to double-check your application for any errors or omissions. Submission methods vary: you can submit your application online through your state's Medicaid portal or send it by mail. Tracking your application status is important, and you should keep an eye on notifications regarding its progress.
After submission: what happens next?
After you submit your Medicaid managed care reenrollment form, there will be a processing period during which your application will be evaluated. Expect notifications regarding the status of your reenrollment, which may include reinstatement or denial notifications. If issues arise, it’s essential to address them promptly to avoid any lapse in your Medicaid coverage.
Tools and resources to aid your reenrollment
Leverage interactive tools such as those available on pdfFiller to assist in filling out and managing your Medicaid managed care reenrollment form. Icons and tutorials can guide you through the upload and completion process, while online resources at your state’s Medicaid website can provide the latest updates and necessary information. Lastly, don’t hesitate to reach out to your state Medicaid office for specific inquiries.
Frequently asked questions about Medicaid managed care reenrollment
Many individuals have common questions regarding the reenrollment process. For instance, if you miss the deadline, you may face a lapse in coverage. If that happens, you can still apply for Medicaid, but eligibility will depend on your income at the time of reapplication. Additionally, during reenrollment, you can opt to switch your managed care provider if desired. Lastly, if you're denied reenrollment, you have the right to appeal the decision, and understanding that process is crucial.
Related topics and guides
For further understanding, consider delving into related topics such as the differences between Medicaid and CHIP, how to appeal Medicaid decisions, and other resources available for Medicaid recipients. Gaining a broader perspective can help maximize your benefits and ensure you have the most up-to-date information available.
Interactive features on pdfFiller
pdfFiller offers seamless options for editing and eSigning your Medicaid managed care reenrollment form. The platform enables collaboration with family members, ensuring everyone involved can have input before submission. Moreover, by utilizing its cloud-based document management, you can access your forms from anywhere, ensuring you never miss a deadline.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I edit medicaid managed care reenrollment in Chrome?
How do I fill out the medicaid managed care reenrollment form on my smartphone?
Can I edit medicaid managed care reenrollment on an Android device?
What is medicaid managed care reenrollment?
Who is required to file medicaid managed care reenrollment?
How to fill out medicaid managed care reenrollment?
What is the purpose of medicaid managed care reenrollment?
What information must be reported on medicaid managed care reenrollment?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.