Get the free considering equity in clinical trials for highlighting impact ...
Get, Create, Make and Sign considering equity in clinical
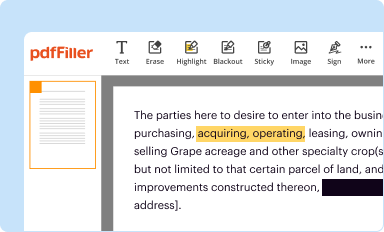
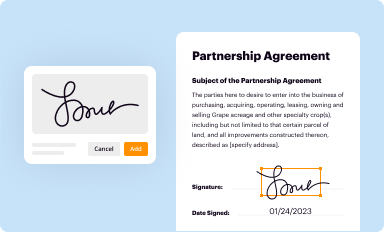
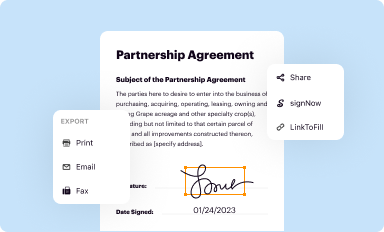
Editing considering equity in clinical online
Uncompromising security for your PDF editing and eSignature needs
How to fill out considering equity in clinical
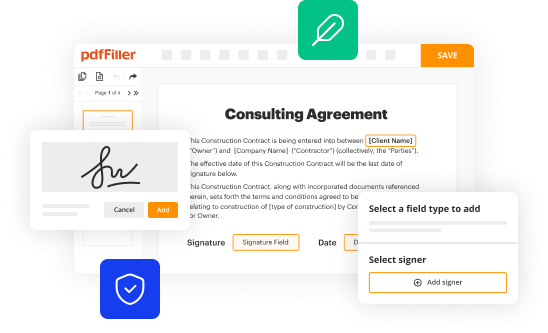
How to fill out considering equity in clinical
Who needs considering equity in clinical?
Considering equity in clinical form
Understanding the concept of equity in healthcare
Equity in healthcare refers to the principle that everyone should have fair access to health services, regardless of their socioeconomic status, geographic location, or personal circumstances. More than just providing equal care, healthcare equity seeks to address the systemic disparities that prevent certain groups from achieving optimal health outcomes.
Historically, the evolution of healthcare equity can be traced back to civil rights movements of the mid-20th century which demanded equal treatment in various public sectors, including healthcare. Over decades, policies and legislation such as the Affordable Care Act have aimed to rectify longstanding inequities. Key principles of healthcare equity include justice, inclusivity, and respect for diversity. These principles guide the creation and implementation of healthcare policies and practices.
The importance of equity in clinical forms
Equitable clinical forms are critical components of a fair healthcare system. They serve not only as documents for patient information but also as tools that can significantly impact patient outcomes. For instance, well-designed clinical forms can reduce barriers to access, enabling timely and appropriate care for all patients. Conversely, inequities in clinical documentation can result in misdiagnoses or delayed treatments, disproportionately affecting vulnerable populations.
Moreover, there are legal and ethical imperatives to ensure that clinical documentation practices uphold equity. Failure to do so can lead to violations of patient rights and ultimately compromise the trust between healthcare providers and patients. Clinical forms play a pivotal role in streamlining communication between patients and providers, which is key to equitable healthcare delivery. By critically analyzing and improving these forms, healthcare systems can promote fair access to necessary care.
Identifying disparities in clinical forms
Health disparities manifest in various forms, from differences in access to care based on income and ethnicity to variances in treatment outcomes. Common health disparities include higher rates of chronic illnesses such as diabetes and hypertension among low-income communities and racial minorities. Understanding these disparities is vital when identifying how they affect clinical documentation processes.
Socioeconomic status often dictates the quality of healthcare that individuals receive, and this is reflected in clinical forms. For instance, patients from low-income backgrounds may encounter more complex language and inadequate resources while filling out clinical documents. Case studies reveal that disparities in clinical workflows, such as appointment availability and follow-up care, often coincide with the challenges posed in clinical forms, creating a compounded effect of inequity.
Social determinants of health in clinical settings
Social determinants of health (SDOH) are the conditions where individuals are born, live, learn, work, and play that affect their health outcomes. These factors can include socioeconomic status, education, neighborhood and physical environment, employment, social support networks, as well as access to healthcare. Recognizing SDOH is essential for creating equitable clinical environments.
In clinical settings, social determinants can influence how accessible clinical forms are to patients. For instance, language barriers can prevent non-English speaking patients from filling out forms accurately. Strategies to address these determinants include hiring multilingual staff, providing forms in various languages, and designing clear visual instructions for completing documentation. By fostering an environment where all patients can engage with clinical forms, healthcare providers can promote fairer health outcomes.
Best practices for creating equitable clinical forms
Creating equitable clinical forms begins with thoughtful design considerations aimed at inclusivity. Language accessibility is paramount; using simple, straightforward language helps ensure all patients can comprehend the questions being asked. Additionally, employing cultural sensitivity in questions and instructions can significantly enhance the ability of diverse populations to complete forms accurately.
Moreover, anonymizing data on these forms can protect vulnerable populations from potential discrimination, ensuring that their health information remains confidential. Involving community stakeholders in the design process can further ensure that diverse perspectives are incorporated, leading to forms that resonate with a broader audience. Best practices thus point towards collaboration and iterative feedback to foster adaptability in form design.
Tools for measuring equity in clinical documentation
To effectively measure equity in clinical forms, healthcare organizations should employ various metrics aimed at gauging accessibility and outcomes. Assessing metrics can include analyzing patient completion rates of forms across demographics and identifying disparities in treatment outcomes based on documented information.
Surveys and feedback mechanisms are valuable tools for gathering insights directly from patients. This feedback can highlight areas needing improvement within clinical documentation processes. Moreover, data analysis can reveal trends and gaps in the documentation that perpetuate inequities, guiding future improvements.
Implementing equity in clinical workflows
Training staff on equity principles is crucial to implementing effective change within clinical workflows. Staff education should cover implicit biases, cultural competence, and the importance of equitable practices in patient care. By fostering a culture of equity within healthcare teams, organizations can improve patient interactions and increase the overall quality of care.
Moreover, establishing clinical governance that prioritizes equity ensures that healthcare organizations maintain accountability. Collaboration among providers is essential to identify best practices and share resources that promote equitable care delivery. An integrated approach not only benefits patients but also enhances organizational performance.
Challenges to achieving equity in clinical forms
Despite the clear advantages of considering equity in clinical forms, numerous challenges can hinder progress. Resistance to change within institutions is a significant barrier; many organizations may take a long time to adapt to new practices due to entrenched customs and institutional inertia.
Technological barriers also pose challenges, particularly regarding access and adoption of innovative solutions. Smaller practices may lack the resources to invest in advanced clinical form software that facilitates equity. Additionally, ethical dilemmas can arise when implementing equity measures, especially surrounding data privacy and the need to balance equity with efficiency.
Navigating regulatory and ethical considerations
Amid the push for equity in healthcare, several regulations have emerged to support these initiatives. Legislation such as the Health Insurance Portability and Accountability Act (HIPAA) establishes frameworks for patient privacy, while other federal and state laws demand transparent documentation practices. Compliance with these regulations is essential for achieving equity.
Ethical reviews can support equitable practices by examining the implications of policies and procedures on diverse patient populations. Institutional Review Boards (IRBs) play a crucial role in ensuring that equity assessments are integrated into research protocols, enabling a holistic consideration of equity in healthcare delivery.
Innovative solutions to enhance equity in clinical forms
To address the challenges of equity in clinical forms, innovative solutions are critical. Integrating technology, such as electronic forms that include accessibility features, can dramatically improve the efficiency of clinical documentation. For example, forms with adaptive design for visually impaired patients enhance usability, ensuring that everyone has equal opportunities to participate in their care.
Community engagement programs can also bolster efforts to promote equity by educating patients on how to navigate clinical forms effectively and providing assistance as needed. Real-world examples of successful initiatives include outreach programs that train community health workers to provide support to low-income patients, which significantly improve completion rates of clinical forms.
The future of equity in clinical documentation
As healthcare continues to evolve, so too do the conversations around equity and clinical documentation. Emerging trends, such as the rise of patient-centered care models, are increasingly recognizing the importance of addressing equity at foundational levels. Innovations in clinical form design—like customizable templates that adapt to individual needs—promise to improve accessibility in equitable practices.
The future will increasingly rely on data analytics to inform equity strategies. By fostering a culture of continuous improvement, healthcare organizations can remain agile in their efforts to identify and mitigate disparities. Embracing equity as a core value will drive organizations forward towards a more just healthcare system.
Case studies highlighting successful equity practices
To better understand the real-world application of equity in clinical practices, it's valuable to examine successful case studies. For instance, the Massachusetts Department of Public Health’s Equity Initiative implemented tailored clinical forms that addressed language barriers, resulting in a noticeable increase in patient engagement among non-English speaking populations.
Likewise, notable healthcare providers have partnered with community organizations to co-create clinical forms that reflect the needs of underrepresented communities. These collaborative approaches are not only effective in improving healthcare access but also serve as a model for other organizations striving to enhance equity in their practice.
Engaging in the equity conversation
Engaging in meaningful conversations about equity is vital for fostering awareness and driving change in healthcare systems. Various forums and platforms exist for healthcare professionals, patients, and advocates to discuss these topics. Networking events, webinars, and community outreach programs are excellent venues for sharing insights and strategies around equity.
Promoting awareness through education is equally important; information campaigns can help community members understand their rights regarding healthcare access. By actively participating in the equity conversation, stakeholders can leverage collective knowledge to address systemic issues and advocate for policies that elevate equity in clinical documentation.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
Can I sign the considering equity in clinical electronically in Chrome?
How do I edit considering equity in clinical straight from my smartphone?
How do I edit considering equity in clinical on an iOS device?
What is considering equity in clinical?
Who is required to file considering equity in clinical?
How to fill out considering equity in clinical?
What is the purpose of considering equity in clinical?
What information must be reported on considering equity in clinical?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.