Get the free Request for Prior Authorization for Stimulant Medications
Get, Create, Make and Sign request for prior authorization



Editing request for prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out request for prior authorization

How to fill out request for prior authorization
Who needs request for prior authorization?
A comprehensive guide to the request for prior authorization form
Understanding prior authorization
Prior authorization is a critical component of modern healthcare systems, primarily serving as a tool for insurance providers to manage costs and ensure that specific treatments or services are medically necessary. This process involves obtaining approval from an insurance company before certain procedures, medications, or services are provided to ensure that they meet the insurer's criteria for coverage. The essence of prior authorization lies not just in cost management, but also in patient safety, ensuring that patients receive appropriate care without unnecessary financial burdens.
In healthcare, prior authorization is often required for various scenarios, particularly those involving high-cost medications, specialized treatments, or new technologies. For instance, a patient seeking a specific MRI or an expensive medication for a chronic condition like rheumatoid arthritis usually faces a need for prior authorization. This requirement aims to prevent misuse of resources, which can lead to higher healthcare costs for both insurers and ultimately for consumers.
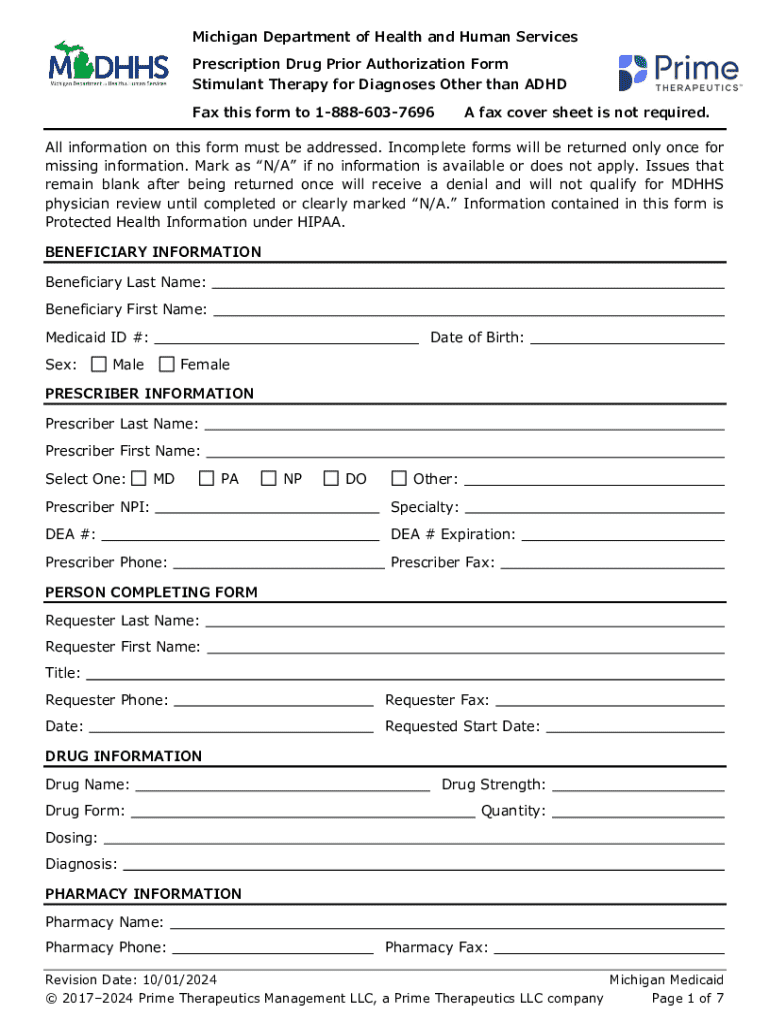
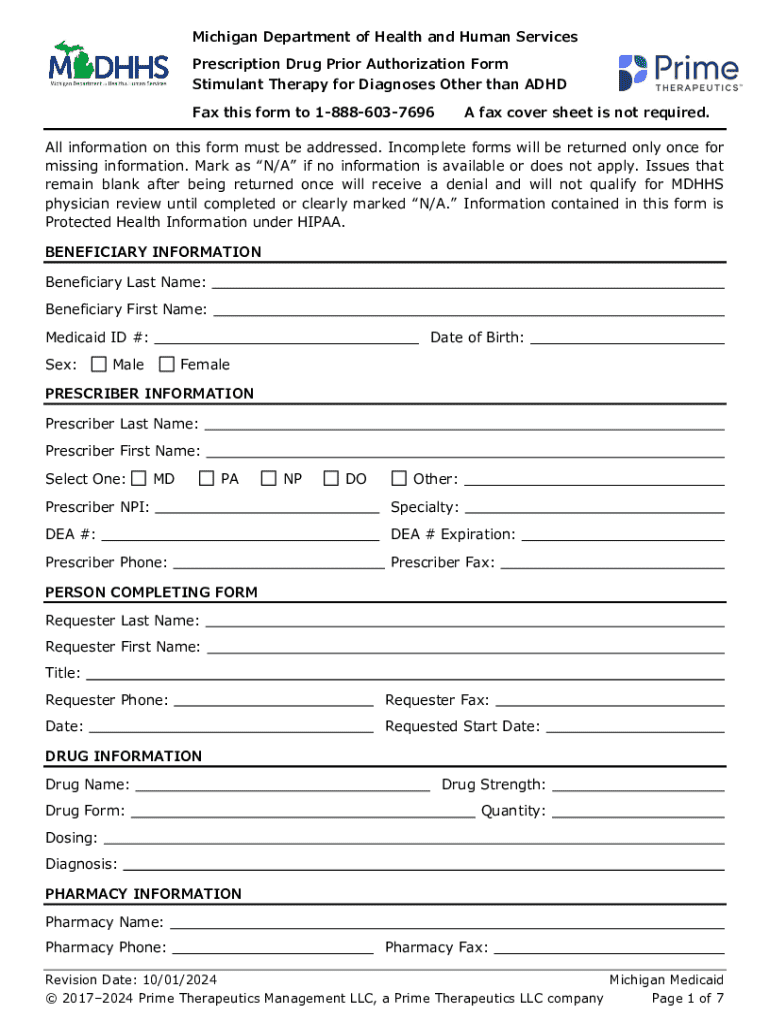
The prior authorization form: an overview
The request for prior authorization form is a standardized document that collects essential information regarding a patient, the healthcare provider, and the specific service being requested. It's vital to provide comprehensive and accurate information on the form to avoid delays in treatment or denial of the request. The core components typically include patient demographics, provider details, and a clear description of the procedure or treatment, including supporting medical history.
When completing the form, certain common mistakes can hinder the process. Missing information, such as incorrect patient identification or provider signatures, can lead to automatic denials. Additionally, a lack of justification for medical necessity often results in requests being turned down, as insurers need to establish that the requested service is essential for the patient’s health. Using incorrect medical coding can also cause delays or denials, making accuracy crucial.
How to obtain the prior authorization form
Obtaining the request for prior authorization form typically involves checking your insurance provider's website or contacting their customer service directly. Many insurers now offer downloadable forms on their websites, making the process easier for both patients and providers. Navigating the insurance provider's website usually requires finding the 'Forms' or 'Prior Authorization' section, where you can directly access the necessary documentation.
If you're unable to access the form online, calling your insurance provider is another option. When reaching out to customer service, it’s helpful to have the following information ready: your insurance policy number, the patient's date of birth, and any specific questions about the authorization process. This prepared approach helps streamline the conversation and ensures you receive all required information.
Filling out the prior authorization form
Completing the request for prior authorization form requires attention to detail to ensure that all relevant information is clearly communicated. Start by gathering necessary patient data such as their name, insurance policy number, and contact information. Next, enter the healthcare provider's information, including the NPI number, specialty, and contact details. Clearly articulate the service or treatment being requested, providing thorough descriptions along with any relevant codes if needed.
Documentation to support the medical necessity of the request can include historical treatment records, recent test results, or clinical notes. Providing these will facilitate a smoother authorization process. After completing the form, take time to review for completeness and accuracy; utilizing validation tools available online can help verify that all data aligns with insurance requirements to prevent unnecessary delays.
Common challenges and solutions
Many individuals encounter challenges when navigating the prior authorization process, including delays in processing and approvals. Understanding that typical turnaround times can range from a few days to several weeks is crucial. If an authorization isn’t received promptly, contacting the insurer to inquire about the status can often expedite the process. Documentation of all interactions is helpful, providing a record of your efforts to secure the necessary approvals.
Denials also pose a significant hurdle in the prior authorization process. Denials occur for various reasons, such as lack of medical necessity or incorrect information on the form. If a submission is denied, the first step should be to carefully review the insurer's explanation, which often outlines the reasons for the denial. If the justification seems inadequate, appealing the decision with additional documentation or clarification can greatly enhance your chances of a successful outcome.
Interactive tools and resources
Receiving assistance during the paperwork process for the request for prior authorization can vastly improve efficiency. One useful tool is pdfFiller’s document management features that allow users to fill, edit, and eSign forms with ease. Utilizing pdfFiller empowers individuals and teams to collaborate in real-time, ensuring all necessary adjustments are completed on one platform. The cloud-based nature of this service means you can access your documents from anywhere, enhancing your workflow.
Additionally, leveraging pre-existing templates makes form submission not only efficient but also ensures compliance with insurer-specific requirements. With pdfFiller, customizing these templates to meet your specific needs is straightforward, allowing for a tailored approach when submitting requests. This adaptability can substantially streamline the process and reduce the likelihood of submission errors.
FAQs about prior authorization
Navigating the labyrinth of prior authorization can lead to many questions from patients and providers alike. One common query is, 'What happens after submission?' Typically, the insurance provider will review the request and notify both the patient and provider of the decision. Timelines can vary, so staying proactive about following up is essential.
Another frequent question concerns the duration of prior authorizations. Generally, these approvals remain valid for a specified period, often from 30 to 90 days, but this can vary by insurer. Lastly, patients sometimes wonder if they can directly request their prior authorization. While patients can initiate the process, working closely with their healthcare providers is usually more effective to ensure that all necessary documentation is submitted accurately.
Real-life examples and case studies
Real-life examples illustrate the value of effectively navigating the request for prior authorization process. One patient, after experiencing a significant delay in treatment for a herniated disk, successfully expedited their MRI approval by providing comprehensive documentation of prior treatments and physician notes that highlighted the urgency of the condition. This proactive approach led to a quicker resolution, showcasing the importance of clear communication and thorough documentation.
Another case involved a complex medication regimen for a cancer treatment. The healthcare provider utilized the request for prior authorization form with detailed medical history and justification of the treatment's necessity, resulting in rapid approval. These instances emphasize that thorough preparation and understanding of the process can lead to successful outcomes, ultimately helping patients receive the care they need without unnecessary delays.
Final thoughts on managing your prior authorization needs
Staying organized is vital for successfully managing prior authorization requests. Keeping detailed records of submitted forms, approvals, and provider communications can help reduce stress during what is already a complex process. Utilizing tools such as calendar reminders can also aid in tracking renewal deadlines to ensure there are no interruptions in coverage.
Embracing technology plays a crucial role in document management. The use of a platform like pdfFiller not only enhances the ease of form completion but also improves collaboration between patients and providers, ensuring smooth processing of prior authorizations. The cloud-based nature of such tools allows users to maintain access to important documents from anywhere, making the entire process far more manageable, organized, and efficient.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I send request for prior authorization to be eSigned by others?
Can I create an electronic signature for the request for prior authorization in Chrome?
Can I create an electronic signature for signing my request for prior authorization in Gmail?
What is request for prior authorization?
Who is required to file request for prior authorization?
How to fill out request for prior authorization?
What is the purpose of request for prior authorization?
What information must be reported on request for prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.