Get the free Glucagon-like Peptide-1 Prior Authorization Fax Form
Get, Create, Make and Sign glucagon-like peptide-1 prior authorization
How to edit glucagon-like peptide-1 prior authorization online
Uncompromising security for your PDF editing and eSignature needs
How to fill out glucagon-like peptide-1 prior authorization
How to fill out glucagon-like peptide-1 prior authorization
Who needs glucagon-like peptide-1 prior authorization?
A Comprehensive Guide to the Glucagon-Like Peptide-1 Prior Authorization Form
Understanding glucagon-like peptide-1 (GLP-1) therapies
Glucagon-like peptide-1 (GLP-1) therapies, such as liraglutide and semaglutide, are innovative medications designed primarily for the management of type 2 diabetes. These medications work by mimicking the incretin hormones that the body produces naturally to lower blood sugar levels. GLP-1 therapies not only help with glycemic control but also promote weight loss, making them a dual-purpose solution for many patients. However, the adoption of these therapies often comes with barriers, including the requirement for a prior authorization to ensure that the healthcare provider meets specific criteria and justifications.
Prior authorization is an essential process that ensures medical necessity and adherence to insurance coverage guidelines before patients can access GLP-1 medications. It helps streamline the treatment process and limits unnecessary medication prescriptions. To qualify for these therapies through insurance, various eligibility criteria must be met, including having a diagnosis of type 2 diabetes and show evidence of previous treatments or lifestyle changes that were ineffective in managing their condition.
The role of the prior authorization form
A prior authorization form is a document submitted to health insurance companies, requesting approval for specific medications or treatments. In the case of GLP-1 therapies, this form is vital as it provides necessary information about the patient’s history, the prescribing physician's details, and clinical justification for the therapy. The prior authorization form is integrated into the treatment process, serving as a gateway that ensures patients receive the right medications without unnecessary delays.
While it’s easy to confuse prior authorization with other forms of insurance approvals, they are distinct. Prior authorizations focus specifically on the need for a particular service or drug, whereas other approvals could relate to broader treatment plans. This specificity makes the GLP-1 prior authorization form a crucial element in securing timely treatment for diabetic patients.
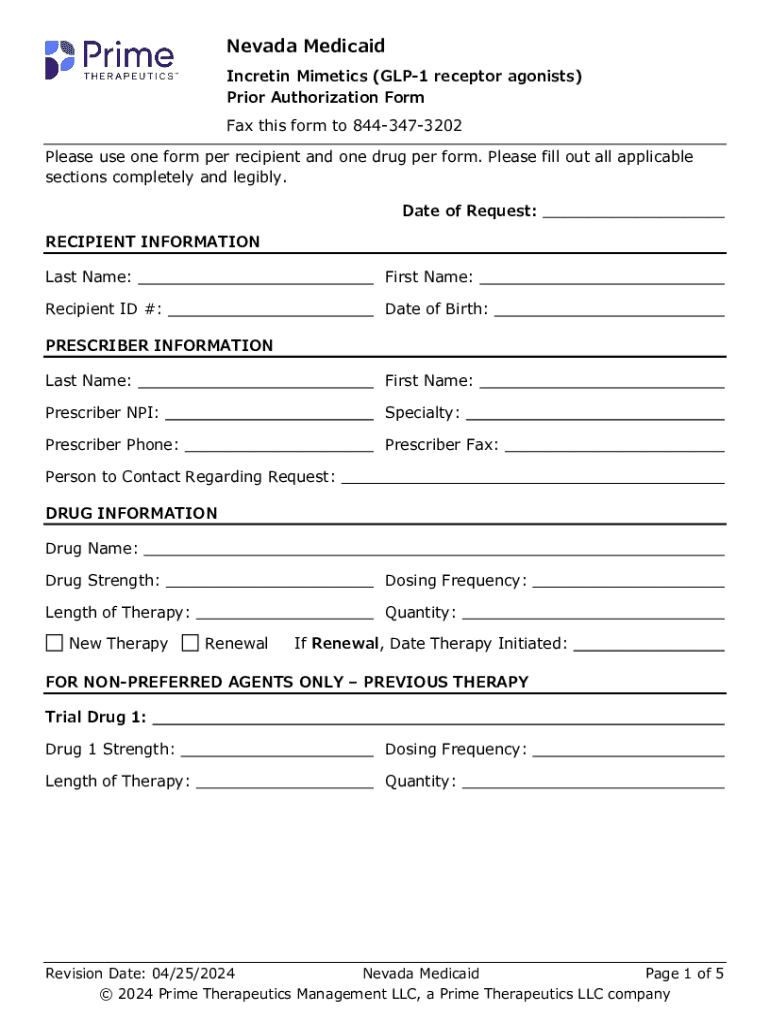
Accessing the GLP-1 prior authorization form
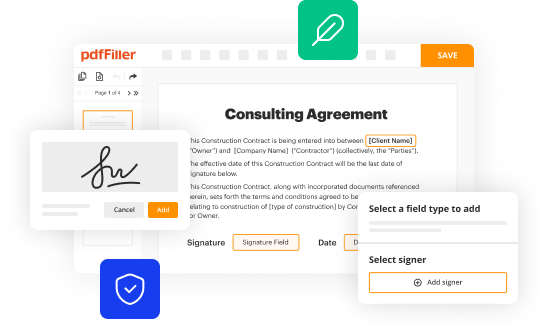
To access the GLP-1 prior authorization form through pdfFiller, you’ll start by visiting the pdfFiller website. pdfFiller offers an interactive platform that simplifies the process of finding and filling out necessary documents. Once on the homepage, utilize the search function to look for 'GLP-1 prior authorization form'. This feature will direct you to the correct template.
Navigating pdfFiller can be straightforward if you know what to look for. Look for tags like ‘Prior Authorization’ or 'Diabetes Management' in the document section. Once you locate the form, open it to understand its format and required fields. This preparation will ensure that you can fill out the form efficiently and correctly.
Detailed instructions for filling out the GLP-1 prior authorization form
Filling out the GLP-1 prior authorization form requires attention to detail to meet the insurance provider's requirements. The form typically includes several sections that must be filled out accurately, each serving a particular purpose. The primary sections include:
Commonly required documentation may include patient medical history, previous treatment records, and any relevant lab results. Providing this supporting information can significantly enhance the chances of approval. Clear examples of completed sections can provide guidance, making it easier to visualize how to fill out the form correctly.
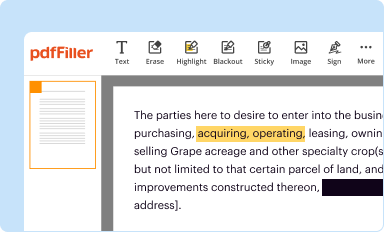
Editing and customizing your prior authorization form
pdfFiller offers various tools that make it easy to edit the GLP-1 prior authorization form. If you find sections that require additional notes or comments, you can easily incorporate these changes using the editing tools available on the platform. Ensuring that your form is clear, precise, and professionally presented can significantly impact the outcome of your submission.
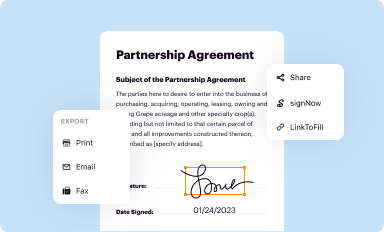
To bolster your document management strategy, utilize pdfFiller's saving and exporting options. After completing the form, you can save it directly to your account or export it in different formats, ensuring easy access and organization of all your healthcare documents.
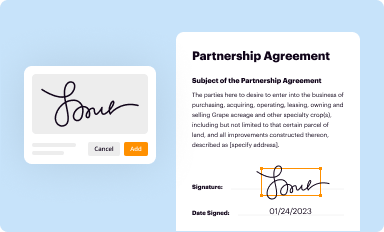
Signing the GLP-1 prior authorization form
Electronic signatures have become increasingly common in healthcare documentation, offering a quick and legally binding way to finalize forms. The GLP-1 prior authorization form can be eSigned easily on pdfFiller's platform. This feature ensures that the documentation is promptly signed, thereby facilitating a quicker submission process.
To eSign your document, simply follow the on-screen prompts, which will guide you through integrating the electronic signature feature. Ensure that any required signatures from prescribers or other necessary parties are also obtained before submitting the form, as incomplete forms can lead to delays or denials.
Submitting the GLP-1 prior authorization form
After completing the GLP-1 prior authorization form, it's time to submit it to the insurance provider. Depending on your insurance company, you may have several methods available for submission, including fax, email, or online portals. Each provider will have specific guidelines regarding how they prefer to receive prior authorization requests.
For best practices, always ensure that you keep copies of what you submit. Tracking submission timelines is also crucial; you should follow up after a week or two if you haven't received a response. Knowing what to expect in terms of approval timelines can help you manage your patient’s expectations more effectively.
Managing your submission and application status
Tracking the status of your prior authorization request is essential to staying informed about its progress. Most insurance providers offer a way to check your application status via their websites or customer service lines. Regular check-ins can help you identify common reasons for denials, such as missing documentation or unmet clinical criteria.
If you encounter a denial, understand the necessary follow-up actions required to rectify the issue. Utilizing pdfFiller's features can aid in document management, allowing you to make updates easily and re-submit anything that may have been overlooked.
Frequently asked questions (FAQs)
Many individuals have inquiries regarding the GLP-1 prior authorization process that may arise. These could include questions about what constitutes medical necessity, how to navigate the appeals process after a denial, and specifics about insurance coverage and reimbursement.
For further assistance, providers can contact their specific insurance companies' helplines or utilize resources from pdfFiller that often include customer service options to resolve common questions efficiently.
Utilizing collaborative tools for teams
Healthcare teams can greatly benefit from using pdfFiller’s collaborative tools when working on prior authorization forms. These tools allow for real-time editing and sharing of documents, ensuring that all members involved in patient care have access to the latest information.
When sharing forms and documents within a team setting, you can do so securely through pdfFiller’s platform, which prioritizes confidentiality and security compliance. Taking advantage of advanced features helps improve project management, tracks progress, and enhances communication among team members.
Case studies: Success stories with GLP-1 prior authorization
Numerous healthcare professionals have experienced success in securing approvals for GLP-1 therapies through diligent prior authorization processes. One notable case involved a patient whose diabetes was poorly controlled despite lifestyle changes; their healthcare provider meticulously documented medical necessity, resulting in swift approval for semaglutide.
These success stories showcase how effectively navigating the prior authorization process can lead to improved patient outcomes. Healthcare providers often learn from previous submissions, refining their strategies and documentation to facilitate easier approvals in the future.
Keeping your forms and documents secure
When handling medical documents, ensuring security and compliance with regulations is of utmost importance. pdfFiller provides features to encrypt documents and maintain compliance with HIPAA guidelines, protecting sensitive patient information at all times.
To further enhance document security, adopt best practices like regularly updating access settings, monitoring shared document activities, and ensuring that all team members understand the importance of confidentiality in handling health data.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I complete glucagon-like peptide-1 prior authorization online?
How do I make edits in glucagon-like peptide-1 prior authorization without leaving Chrome?
How do I fill out the glucagon-like peptide-1 prior authorization form on my smartphone?
What is glucagon-like peptide-1 prior authorization?
Who is required to file glucagon-like peptide-1 prior authorization?
How to fill out glucagon-like peptide-1 prior authorization?
What is the purpose of glucagon-like peptide-1 prior authorization?
What information must be reported on glucagon-like peptide-1 prior authorization?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.