Get the free Nayzilam Prior Authorization Request Form
Get, Create, Make and Sign nayzilam prior authorization request



How to edit nayzilam prior authorization request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out nayzilam prior authorization request

How to fill out nayzilam prior authorization request
Who needs nayzilam prior authorization request?
Understanding the Nayzilam Prior Authorization Request Form
Understanding the Nayzilam prior authorization request form
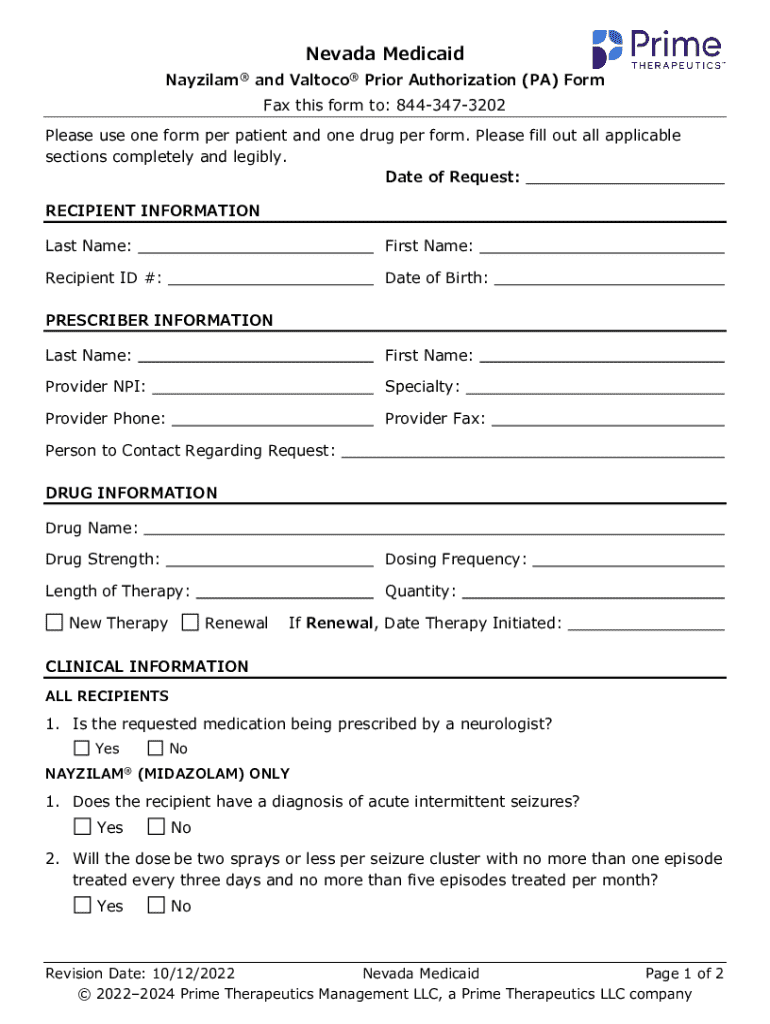
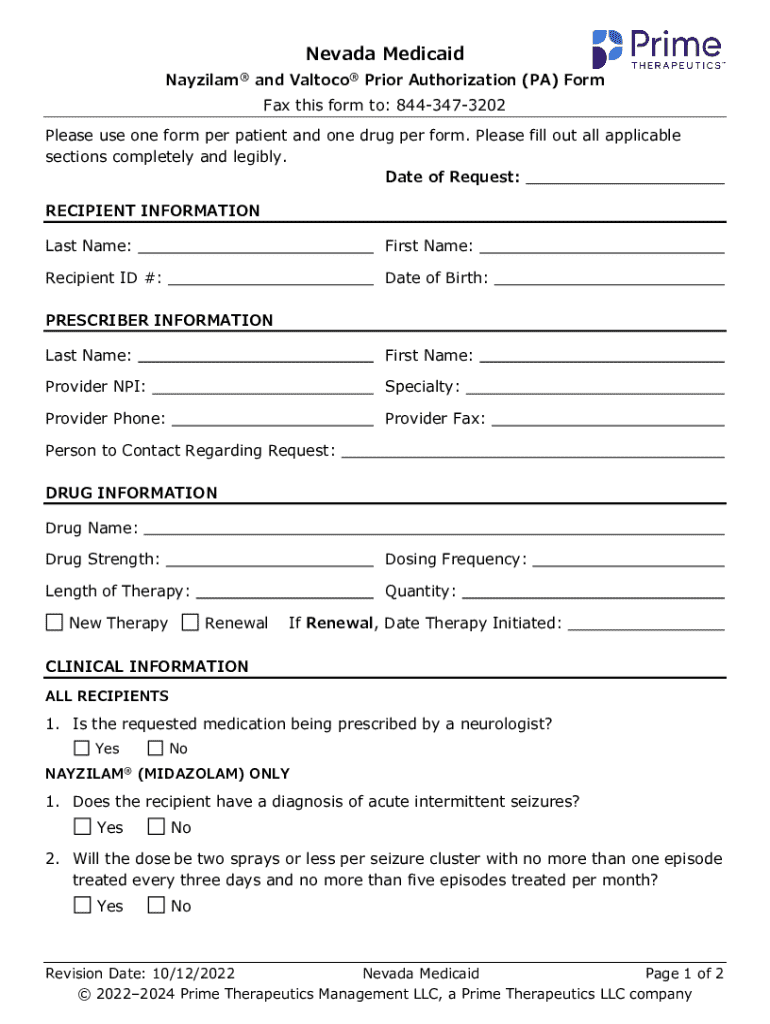
The Nayzilam prior authorization request form is a critical document designed to facilitate the approval process for Nayzilam (midazolam nasal spray), a medication utilized for the acute management of seizures in certain patients. The purpose of this form is to verify the medical necessity of Nyzilam before the prescription can be filled. By requiring prior authorization, insurers aim to ensure that the drug is appropriate for the patient’s unique medical condition, thereby optimizing treatment outcomes and controlling costs.
Prior authorization serves as a safeguard in medication management, protecting patients and healthcare systems alike from unnecessary expenses or inappropriate treatment. It allows healthcare providers to detail the clinical reasoning behind the prescription, ensuring that the patient receives a necessary and proven treatment. This process can prevent the use of ineffective therapies, ensuring that patients receive the most suitable medication for their condition.
Who needs to complete the Nayzilam prior authorization request form?
The Nayzilam prior authorization request form typically requires input from multiple parties. Healthcare providers are often the primary initiators of this form. They fill it out to justify the prescribing of Nayzilam based on the patient's specific health needs. Healthcare providers should be aware of their insurer's guidelines to prepare a comprehensive request.
Patients also play a role in this process. It is essential for patients to understand what the request entails, as they may need to provide personal health information or confirm certain details about their medical history. Strong communication with their provider can empower patients to ensure that all necessary information is available and accurate.
Insurers influence the process by imposing requirements linked to the Nayzilam prior authorization request. Each insurance company may have distinct criteria for approval, impacting how the form is filled out and submitted. Understanding insurer-specific requirements helps streamline the approval process.
Key components of the Nayzilam prior authorization request form
Completing the Nayzilam prior authorization request form requires attention to specific details to ensure a smooth process. The essential sections of the form include various components that gather necessary information for both the patient and provider.
Step-by-step guide to completing the Nayzilam prior authorization request form
Completing the Nayzilam prior authorization request form can be straightforward if the right steps are followed. Here’s how to ensure your submission is thorough and accurate.
How to submit the Nayzilam prior authorization request form
Once the Nayzilam prior authorization request form is complete, it needs to be submitted to the appropriate insurance company. Understanding the submission methods available can streamline this process.
After submission, it’s important to handle confirmation and follow-ups effectively. Expect a response within the insurer's designated timeframe and keep track of any additional information they may request.
Addressing potential issues and delays
Navigating the Nayzilam prior authorization process can sometimes lead to complications. Being aware of common issues and knowing how to address them is advantageous.
If a denial occurs, it is crucial to understand how to appeal. This process typically involves resubmitting the form with additional documentation or clarification to support the need for Nayzilam.
Utilizing pdfFiller for Nayzilam prior authorization request form management
Using pdfFiller enhances the management of the Nayzilam prior authorization request form with its myriad of features that cater to both individual users and teams.
Interactive tools offered by pdfFiller also streamline collaboration features for providers and their teams, making it simple to work on the same document. Additionally, users can access templates and customize forms to fit their specific needs.
Frequently asked questions about the Nayzilam prior authorization request form
As with any formal request process, questions often arise. Here are some of the most common inquiries regarding the Nayzilam prior authorization request form.
Conclusion: ensuring a smooth prior authorization experience
Completing the Nayzilam prior authorization request form may seem daunting, but with accurate information and timely submission, the process can be smooth. It’s essential to maintain ongoing communication with healthcare providers and insurers to navigate any issues that may arise during the approval process effectively.
Emphasizing accuracy and timeliness will contribute to a more efficient experience for both patients and providers, ensuring that patients receive the medications they need without unnecessary delays.






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How do I make edits in nayzilam prior authorization request without leaving Chrome?
How can I edit nayzilam prior authorization request on a smartphone?
How do I edit nayzilam prior authorization request on an Android device?
What is nayzilam prior authorization request?
Who is required to file nayzilam prior authorization request?
How to fill out nayzilam prior authorization request?
What is the purpose of nayzilam prior authorization request?
What information must be reported on nayzilam prior authorization request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.