Get the free Prior Authorization Provider Request Form
Get, Create, Make and Sign prior authorization provider request



Editing prior authorization provider request online
Uncompromising security for your PDF editing and eSignature needs
How to fill out prior authorization provider request

How to fill out prior authorization provider request
Who needs prior authorization provider request?
A comprehensive guide to the prior authorization provider request form
Understanding prior authorization
Prior authorization serves as a critical mechanism in the healthcare landscape. It is a process designed to ensure that certain services, treatments, or medications are deemed medically necessary before a healthcare provider can proceed. This not only promotes appropriate care but also helps manage healthcare costs by preventing unnecessary procedures.
This process often involves coordination between healthcare providers and insurance companies. When a provider makes a request for a service that requires prior authorization, the insurance company reviews the request against established protocols. If approved, the service is covered under the patient’s plan, which typically benefits both parties by fostering transparency and reducing unexpected medical expenses.
Purpose of the prior authorization provider request form
The primary function of the prior authorization provider request form is to facilitate the collection of necessary information required by insurance companies to assess whether a treatment or service is justified. This comprehensive documentation is essential because it potentially expedites the approval process and decreases the likelihood of delays in patient care.
Moreover, the form also aids healthcare facilities in managing costs effectively. By ensuring that only necessary procedures are authorized, the healthcare industry can maintain a focus on patient safety and cost control. This mitigates the risks of excessive spending, allowing resources to be allocated more effectively across various patient care initiatives.
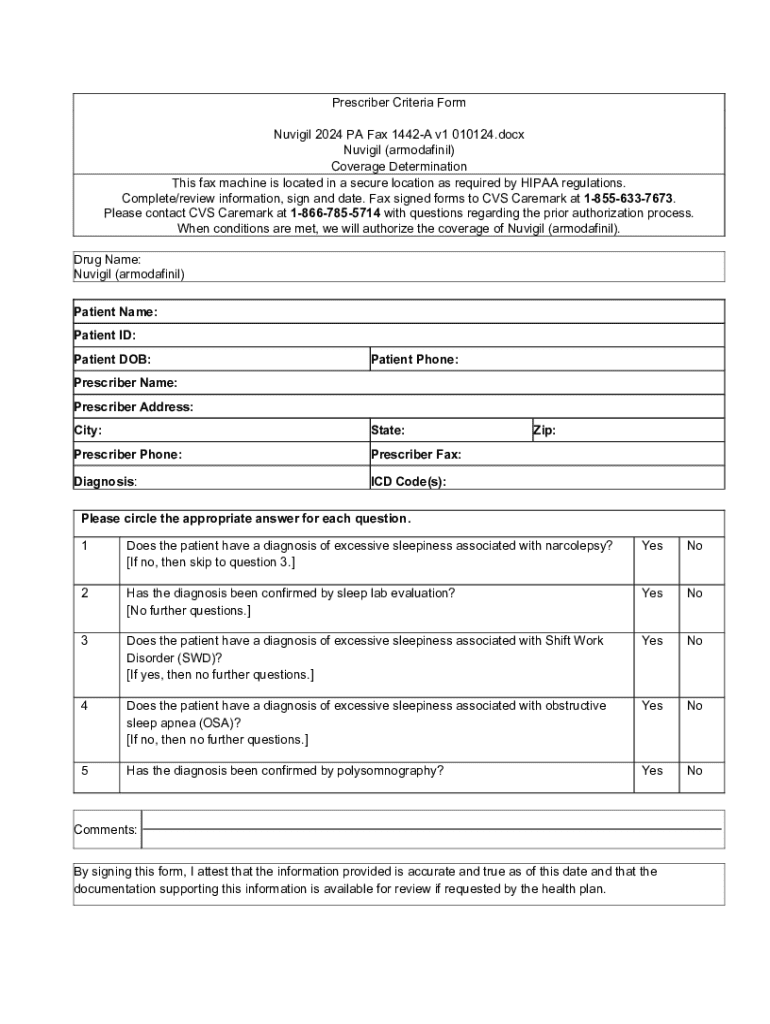
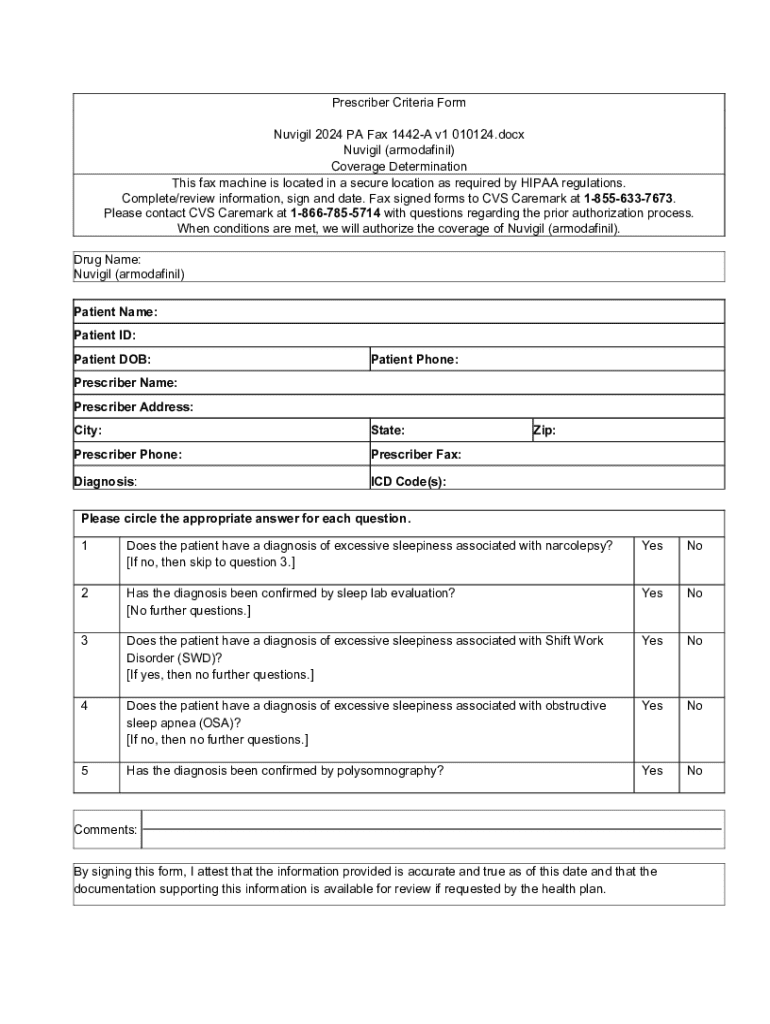
Overview of the prior authorization provider request form
A typical prior authorization provider request form encompasses several critical sections, each contributing to the overall clarity and completeness of the submission. First and foremost are the identification information sections, which include essential patient details and provider information, ensuring that all parties are accurately identified.
Clinical information follows in the form. This section outlines the specific diagnoses and procedures relevant to the request, detailing the reasons for the requested services. The clarity and completeness of this information are vital, as insurance companies are likely to evaluate these details closely during their review process.
Common requirements
Completing the form is not merely an exercise in filling out boxes; it often requires accompanying documentation that supports the requested services. This may include medical records, imaging studies, or other relevant documentation that validates the need for authorization.
Additionally, each insurance provider may have specific requirements that must be adhered to during the completion of the prior authorization provider request form. These guidelines vary depending on the insurer, and understanding them can significantly improve the chances of a swift approval.
Step-by-step guide to filling out the prior authorization provider request form
Filling out the prior authorization provider request form is a structured process that requires attention to detail and thoroughness. The first step is to collect all necessary information about the patient’s medical history, including any previous relevant treatments, diagnoses, and outcomes. This step ensures the form is complete and accurate.
Next is the step of completing the form fields. It’s essential to maintain clarity, using either clear handwriting or typed information to prevent misinterpretation. Nuanced details about the procedures and diagnoses should be articulated precisely to reflect the medical necessity for each requested service.
Finally, review and verify all submitted information. A common mistake is overlooking required signatures or supporting documents, which can lead to delays or denials. Double-checking every element can save valuable time and bolster the approval process.
Editing and managing the form with pdfFiller
Using pdfFiller for document creation streamlines the process of filling out the prior authorization provider request form. Taking the form digital enhances the efficiency of document management, reducing the likelihood of errors commonly associated with paper forms. pdfFiller provides online editing tools that ease the completion process, allowing healthcare teams to work collaboratively even when not physically together.
Additionally, pdfFiller's eSignature integration is crucial for expediting the approval process. The ability to add digital signatures securely validates the documents, ensuring that they are legitimate and ready for submission. This feature also eliminates the need for printing and scanning, making the submission process significantly more efficient.
Submitting the prior authorization provider request
When it comes to submission, providers have the option to submit either digitally or via traditional paper methods. Regardless of the chosen method, it's critical to adopt best practices to ensure accuracy. Keeping a log of submissions, including dates and confirmation numbers, is advisable to track the status and avoid complications down the line.
The follow-up process is another critical aspect. After submitting a request, it's important to stay informed about its status. Most insurance providers will have a method for tracking submissions online. In case of denial, understanding the appeal process is necessary to advocate for the patient’s needs effectively.
Resources for managing authorizations
For those navigating the complexities of the prior authorization provider request form, having access to templates and examples can be invaluable. Sample filled-out forms provide a reference point that ensures completeness and accuracy. Furthermore, having document templates available through pdfFiller can lighten the administrative load by providing structured outlines for various common authorization scenarios.
Interactive tools, such as prior authorization search tools and FAQs, offer quick navigational assistance when users encounter issues. These resources help demystify frequent problems and provide stepwise solutions to common hurdles.
Staying compliant and informed
Navigating prior authorization requirements necessitates an ongoing commitment to compliance and education. The healthcare landscape is constantly evolving, and it's essential for providers to stay abreast of changes in regulations and payer requirements. Accessing resources such as webinars, articles, and industry reports can help maintain an informed status.
Additionally, pdfFiller promotes collaboration among teams through its secure sharing capabilities. This feature ensures that documents are shared only with necessary stakeholders, maintaining confidentiality while enhancing teamwork. As teams collaborate, they can also stay aligned regarding compliance and up-to-date practices.
Simplifying your submission process with pdfFiller
Transitioning to electronic submissions can significantly streamline the prior authorization workflow. The benefits of using pdfFiller extend beyond mere convenience— they encompass cost-effectiveness by minimizing time and resources spent on managing paper documents. The centralized platform allows for seamless document management and reduces the hassles associated with traditional methods.
Should users encounter challenges, pdfFiller offers customer support and assistance to ensure a smooth experience while navigating the various tools and features. Continuous access to community forums and support articles helps users solve issues independently and efficaciously.
Quick links for further support






For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
How can I get prior authorization provider request?
Can I create an electronic signature for signing my prior authorization provider request in Gmail?
How do I edit prior authorization provider request straight from my smartphone?
What is prior authorization provider request?
Who is required to file prior authorization provider request?
How to fill out prior authorization provider request?
What is the purpose of prior authorization provider request?
What information must be reported on prior authorization provider request?
pdfFiller is an end-to-end solution for managing, creating, and editing documents and forms in the cloud. Save time and hassle by preparing your tax forms online.