Get the free COBRA Notice Timing Delivery Chart template
Show details
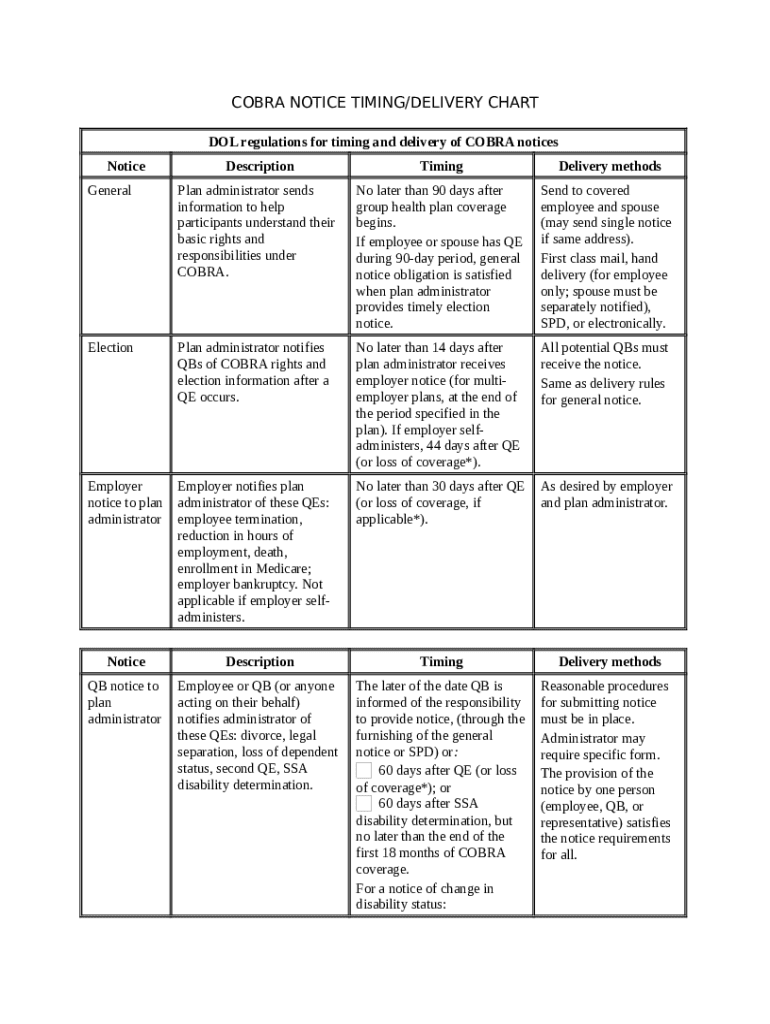
This AHI form is a timing/delivery chart for the Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA).
We are not affiliated with any brand or entity on this form
Why choose pdfFiller for your legal forms?
All-in-one solution
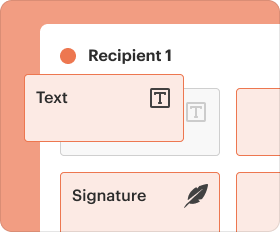
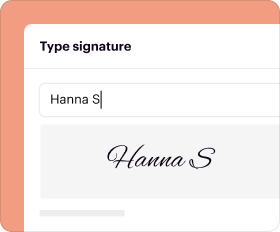
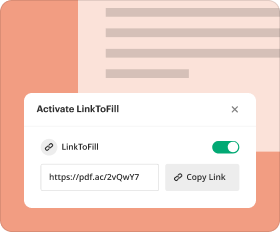
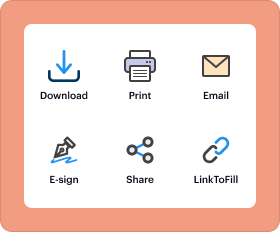
pdfFiller offers a PDF editor, eSignatures, file sharing, collaboration tools, and secure storage—all in one place.
Easy to use
pdfFiller is simple, cloud-based, has a mobile app, and requires no downloads or a steep learning curve.
Secure and compliant
With encryption, user authentication, and certifications like HIPAA, SOC 2 Type II, and PCI DSS, pdfFiller keeps sensitive legal forms secure.
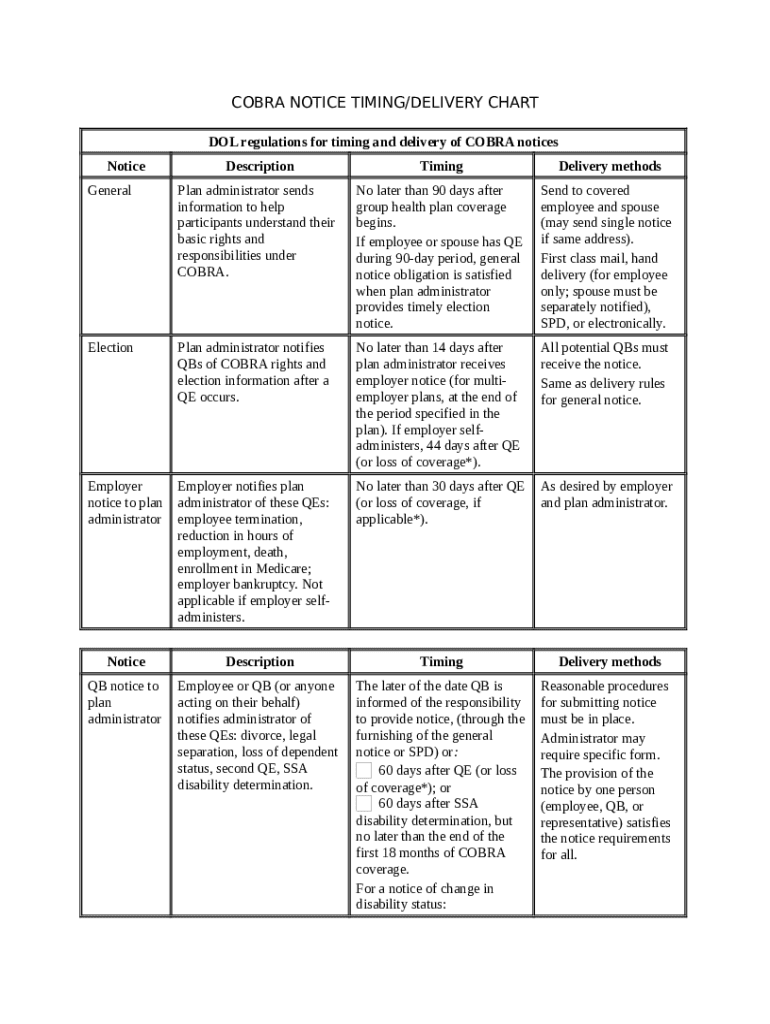
What is cobra notice timing delivery
Cobra notice timing delivery refers to the process and requirements for delivering a COBRA continuation coverage notice to qualified beneficiaries within specific timeframes as mandated by law.
pdfFiller scores top ratings on review platforms




PDF Filler is wonderful
This is a fabulous company and product with all-star customer support! You can't go wrong with PDF Filler!
THIS PROGRAM IS AMAZING ITS SAVED ME SO…
THIS PROGRAM IS AMAZING ITS SAVED ME SO MUCH TIME! EASY TO USE AND GREAT CUSTOMER SERVICE!
review pdfiller use
ok, easy to use, to save
good program
I love this tool
Grate tool
Grate tool, fantastic support team
Who needs cobra notice timing delivery?
Explore how professionals across industries use pdfFiller.
Understanding COBRA Notice Timing and Delivery
How important is timely COBRA notification?
Timely COBRA notifications are critical as they directly impact employee rights regarding health insurance options. Affected individuals need to be informed of their rights and obligations promptly to make informed decisions. Delays can lead to confusion and potential loss of coverage, making timely communication essential for all parties involved.
-
The Consolidated Omnibus Budget Reconciliation Act (COBRA) allows employees and their families to continue health coverage after certain life events, such as job loss or reduction in hours.
-
Employees must receive notifications on time to ensure they can elect coverage without missing deadlines, which is vital for maintaining health benefits.
-
A delay in communication can lead to legal and compliance issues for employers, as it may violate COBRA regulations and put them at risk of penalties.
What is the COBRA notification timeline and employer responsibilities?
Employers have specific responsibilities regarding the timing of COBRA notifications. These responsibilities begin as soon as group health coverage takes effect and vary based on qualifying events.
-
Employers must provide initial COBRA notices within 14 days after the start of coverage, establishing their compliance with federal regulations.
-
The plan administrator must ensure all required notices are sent promptly to eligible participants, ensuring clarity in the coverage being offered.
-
Timelines for notifications can differ depending on the qualifying event, such as termination or divorce, which must be handled within specific time frames to remain compliant.
What are the different types of COBRA notices?
An understanding of the various COBRA notice types is essential for compliance and for informing employees effectively.
-
General Notices must be sent out promptly at the commencement of COBRA eligibility and can be delivered via mail or email, as allowed by regulations.
-
Election Notices inform employees about their rights to choose COBRA coverage and must be delivered within 44 days after a qualifying event.
-
Employers are obligated to send notifications to themselves regarding compliance and must do so within stipulated time frames to adhere to federal guidelines.
How can employers ensure compliance and best practices?
Compliance with COBRA regulations is vital for employers as non-compliance can lead to hefty penalties. Utilizing resources like pdfFiller can greatly facilitate this process.
-
Employers must familiarize themselves with the federal guidelines dictating the details, delivery methods, and timing of all notices.
-
Using automated systems for notifications and regular training sessions can help keep employers up to date with any changes in regulations.
-
pdfFiller offers seamless solutions for creating and sending COBRA forms, ensuring that employers remain compliant while also enhancing communication efficiency.
What should employees do if COBRA notification is delayed?
If employees experience delays in receiving their COBRA notifications, it is crucial that they take immediate action to protect their coverage options.
-
Employees should contact their plan administrator or HR department to inquire about the status of their COBRA notifications.
-
Employers may face legal ramifications and penalties for failing to provide timely notifications, which could have financial repercussions.
-
pdfFiller offers resources for employees needing legal assistance or support regarding COBRA-related questions, ensuring they remain informed.
What interactive tools are available for managing COBRA administration?
Interactive tools can significantly streamline the administration of COBRA requirements, making compliance easier for both employers and participants.
-
pdfFiller's platform includes features that facilitate document creation, organization, and tracking, ensuring proper management of forms.
-
The platform's capabilities allow users to fill out COBRA forms digitally, enhancing efficiency in submission and storage.
-
With collaborative features, teams can work together on documents, ensuring that all necessary requirements are met without misunderstanding.
What qualifying events trigger COBRA notifications?
Identifying qualifying events is crucial for both employers and employees, as these events dictate the timing and necessity of notifications.
-
Common qualifying events include job loss, reduction in hours, divorce, or reaching a dependent age limit.
-
Each event carries different notification requirements, necessitating prompt communication to employees affected.
-
pdfFiller can provide valuable guides and templates to help navigate the complexities surrounding each qualifying event.
How do delivery methods affect COBRA notices?
The method of delivering COBRA notices plays a significant role in compliance and the effectiveness of communication.
-
Employers can choose between mailing physical notices or sending electronic notifications, considering employee preferences and legal compliance.
-
There are specific guidelines for addressing notices to both employees and their dependents, crucial for coverage discussions.
-
Utilizing pdfFiller's platform for electronic documentation ensures that notices are sent swiftly and tracked with ease.
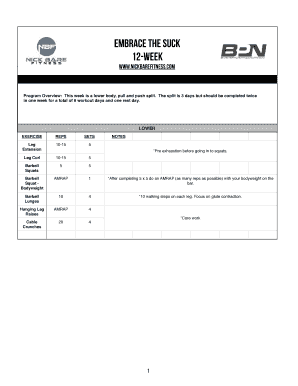
How to fill out the cobra notice timing delivery
-
1.Access pdfFiller and log in to your account.
-
2.Search for 'COBRA Notice Timing Delivery' template in the document library.
-
3.Select the appropriate template and click 'Fill' to start editing.
-
4.Input the relevant employer information at the top of the document, including company name and contact details.
-
5.Enter the names and addresses of qualified beneficiaries who will receive the notice.
-
6.Specify the COBRA coverage options being offered and the relevant time frames for election.
-
7.Fill in the deadlines for notifying beneficiaries about their rights under COBRA.
-
8.Review the completed document for accuracy and ensure all necessary information is included.
-
9.Click 'Save' to store your filled document, or choose 'Print' to send physical copies if necessary.
If you believe that this page should be taken down, please follow our DMCA take down process
here
.
This form may include fields for payment information. Data entered in these fields is not covered by PCI DSS compliance.