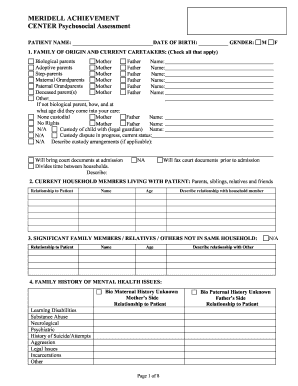
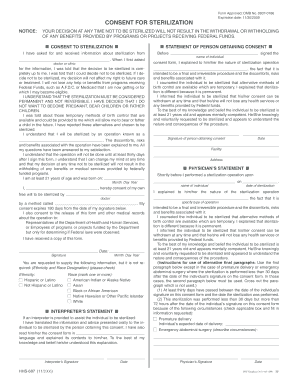
Psychosocial Assessment Form - Page 8
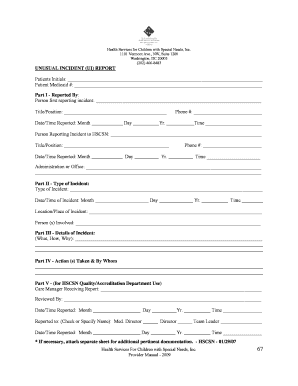
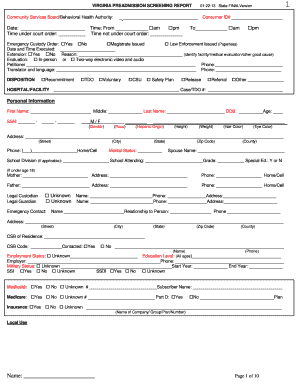
What is the Psychological Assessment Form?
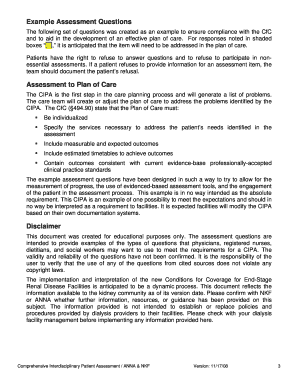
The psychological assessment form is used to record the results of behavioral testing. It consists of a combination of tests, interviews, observations and informal assessment procedures that are used to identify an individual’s emotional and mental state.
It is usually filled out by a medical professional or licensed psychologist. The examination results are used to find out what treatment will work best for the patient. It’s important that this template is filled out with detail and as accurately as possible.
How to Fill Out the Psychological Assessment Form Electronically
To complete this document online, you should drag and drop the existing PDF file. You can also select one of the templates stored in the PDFfiller library. After you have selected the sample in PDF format that best fits your needs, open it and add the following information:
By using up-to-date PDFfiller editor, anyone can fill out the psychological assessment form in just a few minutes and accelerate the document processing time.