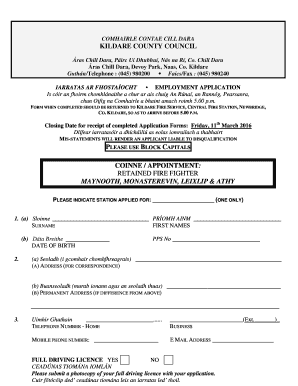
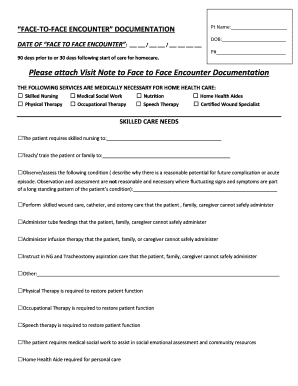
Skilled Nursing Visit Note Form
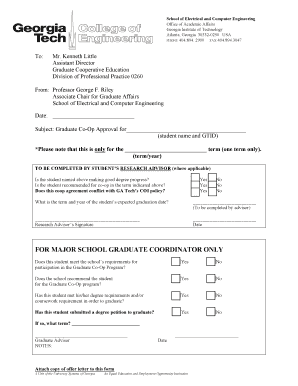
What is skilled nursing visit note form?
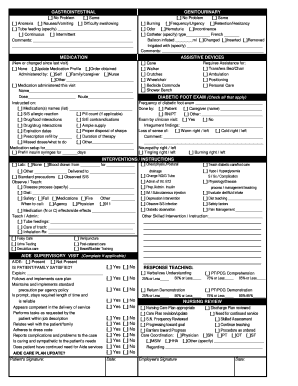
A skilled nursing visit note form is a document used by healthcare professionals to record the details of a patient's visit to a skilled nursing facility. It includes information such as the patient's medical history, vital signs, medications administered, and any observations or assessments made during the visit. This form serves as a crucial tool for maintaining accurate and comprehensive patient records.
What are the types of skilled nursing visit note form?
Skilled nursing visit note forms can vary depending on the specific requirements of the healthcare facility or organization. However, some common types of skilled nursing visit note forms include:
How to complete skilled nursing visit note form
Completing a skilled nursing visit note form requires attention to detail and thorough documentation. Here are some steps to follow:
pdfFiller empowers users to create, edit, and share documents online. Offering unlimited fillable templates and powerful editing tools, pdfFiller is the only PDF editor users need to get their documents done.