Customize and complete your essential Soap Note template
Prepare to streamline document creation using our fillable Soap Note template. Create exceptional documents effortlessly with just a few clicks.
Spend less time on PDF documents and forms with pdfFiller’s tools
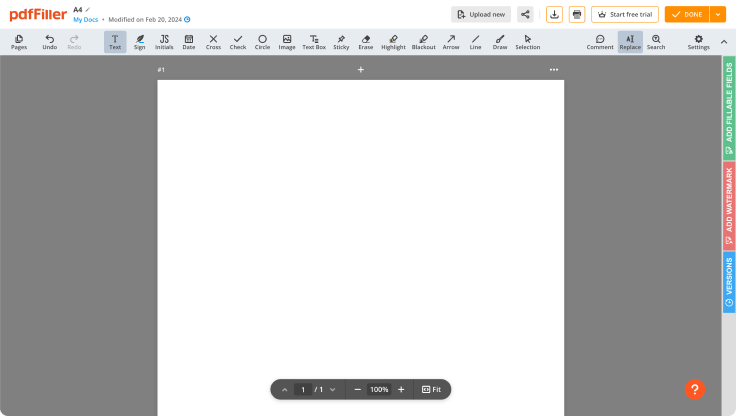
Comprehensive PDF editing
Build documents by adding text, images, watermarks, and other elements. A complete set of formatting tools will ensure a polished look of your PDFs.
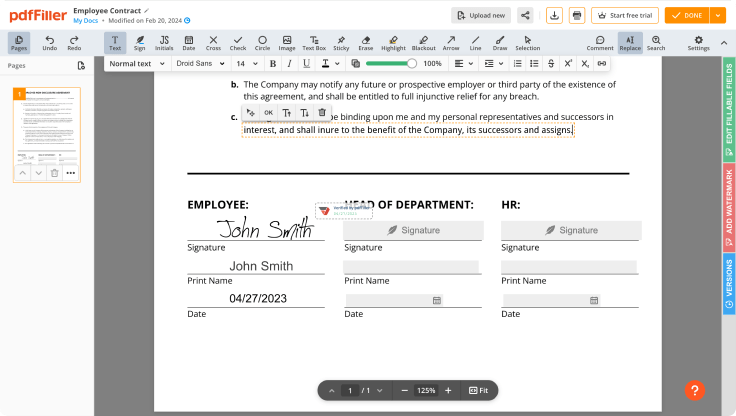
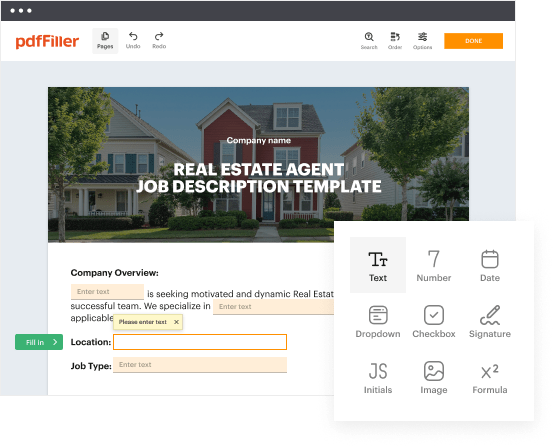
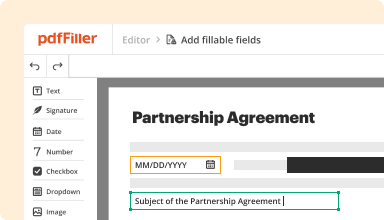
Fillable fields
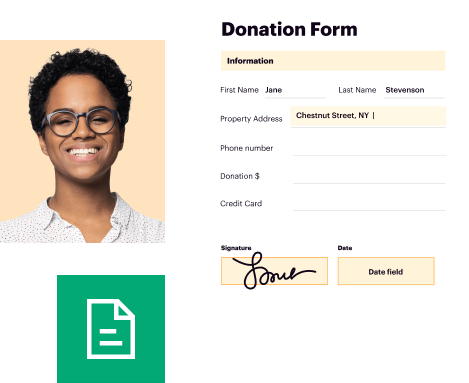
Drag and drop fillable fields, checkboxes, and dropdowns on your PDFs, allowing users to add their data and signatures without hassle.
Templates for every use case
Speed up creating contracts, application forms, letters, resumes, and other documents by selecting a template and customizing it to your needs.
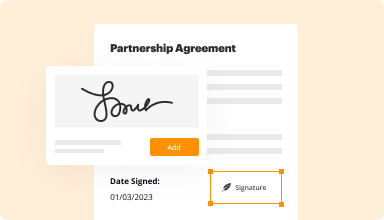
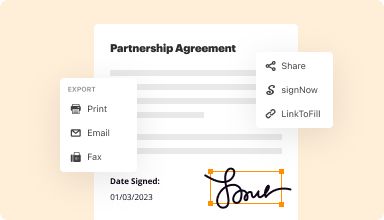
Electronic signature
Instantly sign any document and make it easy for others to sign your forms by adding signature fields, assigning roles, and setting a signing order.
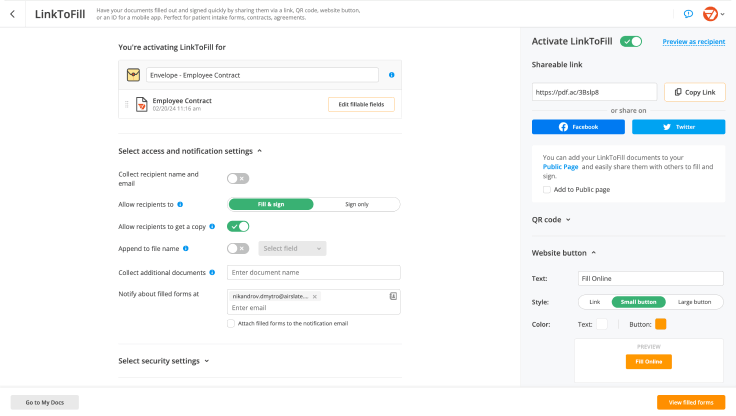
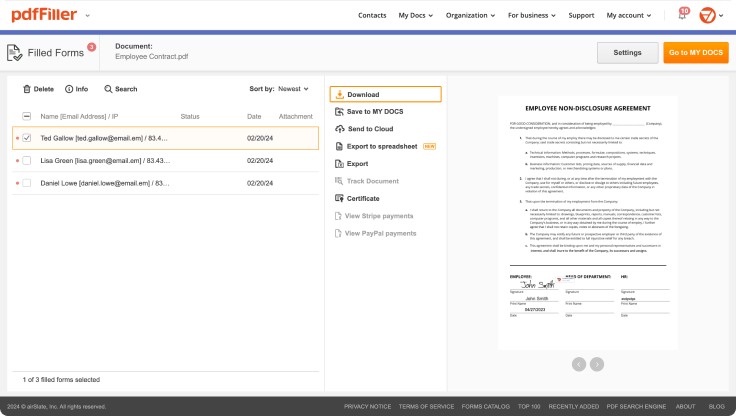
Online forms
Publish fillable forms on your website or share them via a direct link to capture data, collect signatures, and request payments.
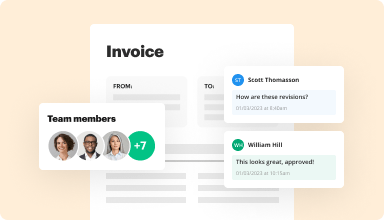
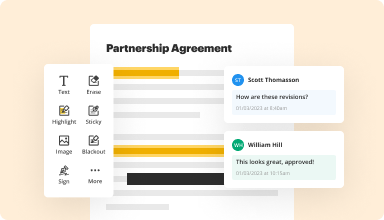
Easy collaboration
Work on documents together with your teammates. Exchange comments right inside the editor, leave sticky notes for your colleagues, highlight important information, and blackout sensitive details.
Millions of users trust pdfFiller to create, edit, and manage documents
64M+
million users worldwide
35M+
PDF forms available in the online library
53%
of documents created from templates
65.5K+
documents added daily
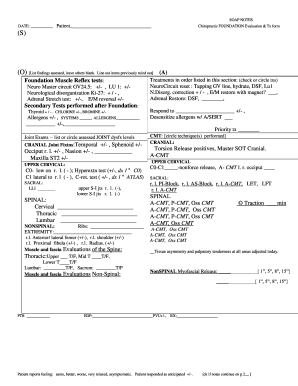
Customize Your Essential Soap Note Template
Create a personalized Soap Note template to streamline your documentation process. This feature allows you to tailor your notes to meet your specific needs, enhancing your workflow and ensuring you capture all necessary information.
Key Features
Easy customization options for layout and content
Templates tailored for different healthcare settings
User-friendly interface for quick adjustments
Option to save and reuse templates
Compatibility with various devices and systems
Potential Use Cases and Benefits
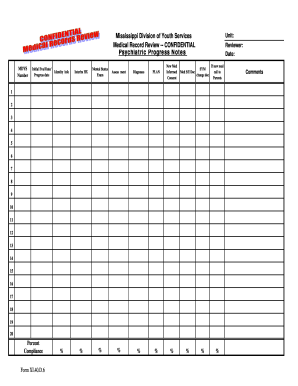
Ideal for healthcare professionals looking to save time on documentation
Supports accurate and consistent record keeping
Enhances patient communication with clear notes
Facilitates team collaboration through standardized notes
Improves compliance with documentation requirements
This tool can significantly reduce the challenges of documentation for healthcare providers. By using a customized Soap Note template, you can ensure that your records are concise, clear, and tailored to your practice. Say goodbye to the frustration of generic templates and welcome a solution that understands your unique needs.
Kickstart your document creation process
Browse a vast online library of documents and forms for any use case and industry.
Top-rated PDF software recognized for its ease of use, powerful features, and impeccable support






Our user reviews speak for themselves
Your go-to guide on how to create a Soap Note
Crafting a Soap Note has never been easier with pdfFiller. Whether you need a professional forms for business or individual use, pdfFiller offers an instinctive platform to create, customize, and handle your paperwork effectively. Use our versatile and fillable web templates that align with your precise requirements.
Bid farewell to the hassle of formatting and manual editing. Utilize pdfFiller to easily create polished forms with a simple click. Begin your journey by using our comprehensive guidelines.
How to create and complete your Soap Note:
01
Create your account. Access pdfFiller by logging in to your account.
02
Search for your template. Browse our comprehensive library of document templates.
03
Open the PDF editor. Once you have the form you need, open it up in the editor and take advantage of the editing tools at the top of the screen or on the left-hand sidebar.
04
Place fillable fields. You can select from a list of fillable fields (Text, Date, Signature, Formula, Dropdown, etc.).
05
Edit your form. Add text, highlight information, insert images, and make any required adjustments. The user-friendly interface ensures the process remains easy.
06
Save your changes. When you are satisfied with your edits, click the “Done” button to save them.
07
Send or store your document. You can deliver it to others to eSign, download, or securely store it in the cloud.
To conclude, creating your documents with pdfFiller templates is a smooth process that saves you efforts and guarantees accuracy. Start using pdfFiller right now to benefit from its robust capabilities and effortless paperwork management.
Ready to try the award-winning PDF editor in action?
Start creating your document in pdfFiller and experience firsthand how effortless it can be.
Questions & answers
Below is a list of the most common customer questions.If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What if I have more questions?
Contact Support
How do you fill SOAP notes?
Tips for Effective SOAP Notes Find the appropriate time to write SOAP notes. Maintain a professional voice. Avoid overly wordy phrasing. Avoid biased overly positive or negative phrasing. Be specific and concise. Avoid overly subjective statement without evidence. Avoid pronoun confusion. Be accurate but nonjudgmental. Tips for Effective SOAP Notes - Purdue OWL Purdue OWL - Purdue University soap_notes soap_note_tips Purdue OWL - Purdue University soap_notes soap_note_tips
What not to put in a progress note?
Information overload: While thoroughness is essential, avoid including irrelevant details. Focus on concise and pertinent information directly related to the patient's condition and treatment plan. Illegible handwriting: If you handwrite notes, ensure they are straightforward to read.
What is an example of a simple SOAP note?
Example 1. Let's look at the following simple SOAP note example. S: Patient states that he did not sleep well last night due to phantom limb pain, RLE; he hopes to take his prosthesis home with him soon so he can use it to walk around the house “like a normal person”. 7. Chapter 07: SIMPLE SOAP NOTE EXAMPLES The Pennsylvania State University psushptamedicaldocumentation The Pennsylvania State University psushptamedicaldocumentation
What not to include in SOAP notes?
Don't make general statements without supporting data: The objective section of your SOAP notes is for hard facts and specific observations. General statements can often lean toward impressions or interpretations. SOAP Note Mistakes to Avoid - ICANotes ICANotes 2021/08/23 soap-note-mist ICANotes 2021/08/23 soap-note-mist
What should not be included in a SOAP note?
Keep reading to learn more! Quick Links: What Are SOAP Notes? Subjective. Objective. Assessment. Plan. Mistake #1: Including statements without supporting evidence. Mistake #2: Using vague language when you could include more details. Mistake #3: Saying the same thing in each of the SOAP note sections.
What are pertinent negatives in a SOAP note?
Pertinent Negatives (PN) are used when the clinician documents why they DID NOT perform a procedure. Example: If Aspirin is part of the agency protocol for Chest Pain but was not administered, the reason should be documented. This is done using PN values.
What are 3 guidelines to follow when writing SOAP notes?
The order in which a medical note is written has been a topic of discussion. While a SOAP note follows the order Subjective, Objective, Assessment, and Plan, it is possible, and often beneficial, to rearrange the order.
How detailed should SOAP notes be?
Despite this variation, it is important to keep in mind that a SOAP note should be sufficiently detailed so that an outside healthcare provider with no previous interaction with the patient/client can obtain all the necessary information from the session or incident documented to appropriately provide care for the SOAP Notes - Healthcare Writing - Purdue OWL Purdue OWL - Purdue University owl subject_specific_writing Purdue OWL - Purdue University owl subject_specific_writing
What are SOAP notes for dummies?
4 components of a SOAP note Subjective. This covers your patient's detailed medical history and current symptoms. Objective. This is a record of your physical examination of the patient's condition. Assessment. The next component of a SOAP note is assessment. Plan. The last component of a SOAP note is the plan.
What does a good SOAP note look like?
SOAP notes include a statement about relevant client behaviors or status (Subjective), observable, quantifiable, and measurable data (Objective), analysis of the information given by the client (Assessment), and an outline of the next course of action (Planning).
How do you write a simple SOAP note?
However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment.
What is a brief SOAP note?
Introduction. The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. The SOAP note is a way for healthcare workers to document in a structured and organized way.[1][2][3]
What tense should a SOAP note be in?
An important part of patient Electronic Health Records, SOAP notes should be legible and make use of professional jargon to serve as a common frame of reference. They should be written in the present tense. Concise and specific.
What goes in each part of a SOAP note?
However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment.
How to fill out SOAP notes for massage?
A massage therapist SOAP note template includes the following information: Client's name and contact information. Date and time of visit. Description of what type of massage was performed. The client's reaction to the massage. Any areas that were sore or felt abnormal before or after treatment.