Put Elect Notice For Free
Drop document here to upload
Up to 100 MB for PDF and up to 25 MB for DOC, DOCX, RTF, PPT, PPTX, JPEG, PNG, JFIF, XLS, XLSX or TXT
Note: Integration described on this webpage may temporarily not be available.
0
Forms filled
0
Forms signed
0
Forms sent
Discover the simplicity of processing PDFs online
Upload your document in seconds
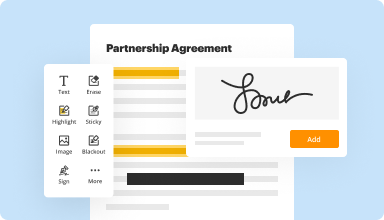
Fill out, edit, or eSign your PDF hassle-free

Download, export, or share your edited file instantly
Top-rated PDF software recognized for its ease of use, powerful features, and impeccable support






Every PDF tool you need to get documents done paper-free
Create & edit PDFs
Generate new PDFs from scratch or transform existing documents into reusable templates. Type anywhere on a PDF, rewrite original PDF content, insert images or graphics, redact sensitive details, and highlight important information using an intuitive online editor.
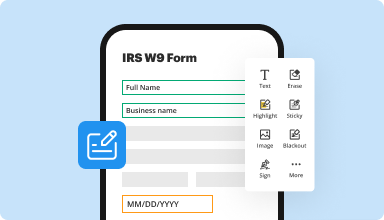
Fill out & sign PDF forms
Say goodbye to error-prone manual hassles. Complete any PDF document electronically – even while on the go. Pre-fill multiple PDFs simultaneously or extract responses from completed forms with ease.
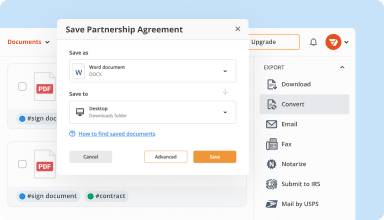
Organize & convert PDFs
Add, remove, or rearrange pages inside your PDFs in seconds. Create new documents by merging or splitting PDFs. Instantly convert edited files to various formats when you download or export them.
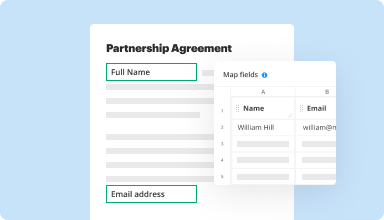
Collect data and approvals
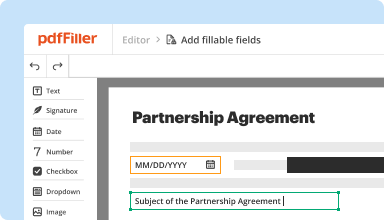
Transform static documents into interactive fillable forms by dragging and dropping various types of fillable fields on your PDFs. Publish these forms on websites or share them via a direct link to capture data, collect signatures, and request payments.
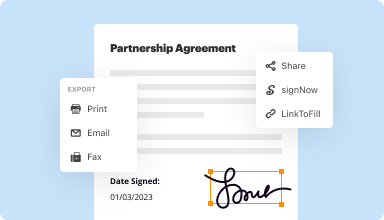
Export documents with ease
Share, email, print, fax, or download edited documents in just a few clicks. Quickly export and import documents from popular cloud storage services like Google Drive, Box, and Dropbox.
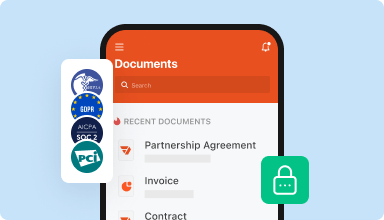
Store documents safely
Store an unlimited number of documents and templates securely in the cloud and access them from any location or device. Add an extra level of protection to documents by locking them with a password, placing them in encrypted folders, or requesting user authentication.
Customer trust by the numbers
64M+
users worldwide
4.6/5
average user rating
4M
PDFs edited per month
9 min
average to create and edit a PDF
Join 64+ million people using paperless workflows to drive productivity and cut costs
Why choose our PDF solution?
Cloud-native PDF editor
Access powerful PDF tools, as well as your documents and templates, from anywhere. No installation needed.
Top-rated for ease of use
Create, edit, and fill out PDF documents faster with an intuitive UI that only takes minutes to master.
Industry-leading customer service
Enjoy peace of mind with an award-winning customer support team always within reach.
What our customers say about pdfFiller
See for yourself by reading reviews on the most popular resources:
What do you like best?
The ablitiy to be able to edit documents in PDF format is great. Saving time. When we are bidding on a job i can use the form provided to us from the client. Very easy to use and has worked well ever time I have neede it. Another great feature is that the PDF filler is auto saved in your online profile... so you can take the documents with you.
What do you dislike?
some times when you go to open the PDF from my email directly... it does not up load... so then I have to down load the pdf on to my computure, open PDF fill web app then upload file..... not sure why it does this but it has happened more often lately than it did before.
Recommendations to others considering the product:
It would be great if the filler could be able to authenticate docuements, a big one for us is Bonding, When we submit a bond they require an e-bonding ( look it up) the ebond authenicates the signatures from 3 different parties and leave a digital paper trail that can be confrimed by the client. We recently had to do this and the one website mobile bonds.com has an interface that is not user freindly for set up... and we had to spend countless time with the tech on the phone for the first few bonds. If the filler is able to do this that would be great.
What problems are you solving with the product? What benefits have you realized?
Allowing us to make our bid proposals look great, avoid hand writing in documents, setting us apart from the rest. we also can share the file with my staff making it even better
The ablitiy to be able to edit documents in PDF format is great. Saving time. When we are bidding on a job i can use the form provided to us from the client. Very easy to use and has worked well ever time I have neede it. Another great feature is that the PDF filler is auto saved in your online profile... so you can take the documents with you.
What do you dislike?
some times when you go to open the PDF from my email directly... it does not up load... so then I have to down load the pdf on to my computure, open PDF fill web app then upload file..... not sure why it does this but it has happened more often lately than it did before.
Recommendations to others considering the product:
It would be great if the filler could be able to authenticate docuements, a big one for us is Bonding, When we submit a bond they require an e-bonding ( look it up) the ebond authenicates the signatures from 3 different parties and leave a digital paper trail that can be confrimed by the client. We recently had to do this and the one website mobile bonds.com has an interface that is not user freindly for set up... and we had to spend countless time with the tech on the phone for the first few bonds. If the filler is able to do this that would be great.
What problems are you solving with the product? What benefits have you realized?
Allowing us to make our bid proposals look great, avoid hand writing in documents, setting us apart from the rest. we also can share the file with my staff making it even better
2019-02-25
What do you like best?
Ease of changing a PDF to suit a particular need and/or make corrections to a PDF to present to a different customers
What do you dislike?
Only downside is not having an autosave when working on a PDF and after being distracted by other people returning to the PDF to find you need to restart.
Recommendations to others considering the product:
Quality solution to alter PDFs to be tailored to suit a particular presentation to a client
What problems are you solving with the product? What benefits have you realized?
Changing PDF's to be tailored and personal as per each individual client that we present to
Ease of changing a PDF to suit a particular need and/or make corrections to a PDF to present to a different customers
What do you dislike?
Only downside is not having an autosave when working on a PDF and after being distracted by other people returning to the PDF to find you need to restart.
Recommendations to others considering the product:
Quality solution to alter PDFs to be tailored to suit a particular presentation to a client
What problems are you solving with the product? What benefits have you realized?
Changing PDF's to be tailored and personal as per each individual client that we present to
2019-04-23
PDF helped me achieve what I had to…
PDF helped me achieve what I had to when signing documents and when I asked for the subscription to be cancelled they obliged which I was thankful for
2020-03-19
Pdffiller: All in one pdf editor
PDFfiller is the most easiest application to create or edit a pdf document.
We can get all the services related to PDF under one roof. We can add a perfect esignature using PDFfiller. Best PDF converter to word file or excel. No need to install any programs to edit PDF.
Pdf filler not support all languages. Doing Page setup and page formatting are little hard. There is no proper backup available for unsaved documents.
2019-08-30
Love the app!
Overall I really like the app and it has been quite useful for me as a realtor =)
Great way to fill out forms and make your own fillable master form.
I have had a hard time figuring out how to easily share and send the form you want and the notifications when you receive it back. Wish I could save the docket in my own files
2019-03-12
Very interesting and helpful as I needed this to hopefully obtain a Passport. My original Certificate is barely readable. Thank you so much, Judith Mann
2023-02-03
This app has been my life saver signing…
This app has been my life saver signing documents for my job and getting them to the right place in a timely manner!
2021-06-29
I would like an easier link in the…
I would like an easier link in the tools to delete sections of PDF/ delete a page in a multi pages document.
2021-04-23
This site made dealing with PDF files…
This site made dealing with PDF files so much easier. Thank you for allowing a free trial during such a trying time in teaching.
2020-04-22
Put Elect Notice Feature
The Put Elect Notice feature streamlines the process of notifying stakeholders about important updates and changes. This tool can enhance communication and ensure everyone is informed efficiently.
Key Features
Automated notification sending to selected contacts
Customizable templates for various notification types
Real-time tracking of notifications
Scheduling options for future notices
User-friendly interface for easy navigation
Potential Use Cases
Notifying employees about policy changes
Updating clients on service modifications
Communicating important deadlines to team members
Announcing product launches to customers
Informing stakeholders of emergency updates
By using the Put Elect Notice feature, you can simplify your communication process, reduce the risk of missed messages, and improve overall efficiency. You can ensure everyone receives timely updates, helping you meet deadlines and maintain strong relationships. This tool is ideal for organizations that value transparency and consistency in their communications.
For pdfFiller’s FAQs
Below is a list of the most common customer questions. If you can’t find an answer to your question, please don’t hesitate to reach out to us.
What if I have more questions?
Contact Support
When must Cobra notices be sent out?
Plan administrators must provide a written general notice of COBRA rights to each covered employee and spouse (if any) within 90 days after their coverage under a GAP begins. The general notice must also be sent to any new dependents added to the plan after the employee's initial enrollment.
How long does an employer have to send out a cobra notice?
The initial notice of rights and benefits in the health plan is required within 90 days of the employee's coverage. If there are changes to the plan, the employer must give notice within 210 days after the year in which the changes take place. If benefits or coverage are being reduced, the notice period is 60 days.
How long does the employer have to send Cobra notice?
Employer has 30 days from the loss of coverage to notify the plan administrator. * Plan Administrator has 14 days to provide a COBRA election notice to the former employee/qualified beneficiary.
What is the penalty for not sending Cobra notice?
Failure to provide the COBRA election notice within this time period can subject employers to a penalty of up to $110 per day, at the discretion of the court, as well as the cost of medical expenses incurred by the qualified beneficiary.
Do Cobra notices have to be mailed?
Notices properly mailed are generally considered provided on the date sent, regardless of whether they're actually received. 1. COBRA Initial Notice must be provided. Within 30 days after the employee first becomes enrolled in the group health plan.
Does Cobra coverage begin immediately?
Assuming one pays all required premiums, COBRA coverage starts on the date of the qualifying event, and the length of the period of COBRA coverage will depend on the type of qualifying event which caused the qualified beneficiary to lose group health plan coverage. In that case, COBRA lasts for 18 months.
When should you get Cobra information?
You must notify the plan, generally within 60 days, if the reason for COBRA eligibility is because of divorce, legal separation or losing dependent status as a child. The health plan then has 14 days to respond with information about how to elect COBRA, and you and your family have 60 days to decide.
How long does an employer have to notify you of Cobra?
Employer has 30 days from the loss of coverage to notify the plan administrator. * Plan Administrator has 14 days to provide a COBRA election notice to the former employee/qualified beneficiary.
#1 usability according to G2
Try the PDF solution that respects your time.






